International Journal of
Environmental Research
and Public Health
Systematic Review
The Psychological and Physical Effects of Forests on Human
Health: A Systematic Review of Systematic Reviews and
Meta-Analyses
Marita Stier-Jarmer 1,2,*, Veronika Throner 1,2, Michaela Kirschneck 1,2, Gisela Immich 1,2, Dieter Frisch 1,2
and Angela Schuh 1,2
1 Public Health and Health Services Research, Institute for Medical Information Processing, Biometry,
and Epidemiology (IBE), Ludwig-Maximilians-Universität München, 81377 Munich, Germany;
vthroner@ibe.med.uni-muenchen.de (V.T.); mkirschneck@ibe.med.uni-muenchen.de (M.K.);
gimmich@ibe.med.uni-muenchen.de (G.I.); dfrisch@ibe.med.uni-muenchen.de (D.F.);
angela.schuh@med.uni-muenchen.de (A.S.)
2 Pettenkofer School of Public Health, Institute for Medical Information Processing,
Biometry and Epidemiology (IBE), Ludwig-Maximilians-Universität München, 81377 Munich, Germany
* Correspondence: mstierj@ibe.med.uni-muenchen.de
Citation: Stier-Jarmer, M.; Throner,
V.; Kirschneck, M.; Immich, G.; Frisch,
D.; Schuh, A. The Psychological and
Physical Effects of Forests on Human
Health: A Systematic Review of
Systematic Reviews and Meta-
Analyses. Int. J. Environ. Res. Public
Health 2021, 18, 1770. https://
doi.org/10.3390/ijerph18041770
Academic Editor: Paul B. Tchounwou
Received: 13 January 2021
Accepted: 2 February 2021
Published: 11 February 2021
Publisher’s Note: MDPI stays neutral
with regard to jurisdictional claims in
published maps and institutional affil-
iations.
Abstract: Background: The aim of this systematic review of systematic reviews was to identify,
summarise, and synthesise the available evidence of systematic reviews (SRs) and meta-analyses
(MAs) on the preventative and therapeutic psychological and physical effects of forest-based in-
terventions. Methods: Both bibliographic databases and grey literature sources were searched
for SRs and MAs published until May 2020. Eight databases were searched for relevant articles:
MEDLINE, Embase, Web of Science, Cochrane Library, PsycInfo, CiNii, EBSCO, and Scopus. Grey
literature was sourced from Google Scholar and other web-based search tools. SRs and MAs that
included randomised controlled (RCT), non-randomised controlled (NRCT), and non-controlled
trials (NCT) on health-related effects of forest-based interventions were eligible if they had searched
at least two databases. The methodological quality of eligible reviews was assessed by AMSTAR-2.
Results: We evaluated 11 systematic reviews covering 131 different primary intervention studies,
mostly from Asian countries, three of which included supplementary meta-analyses. The quality
assessment resulted in moderate confidence in the results of two reviews, low confidence in six, and
critically low confidence in three. The results of the eight moderate and low-rated reviews indicated
that forest-based interventions are beneficial to the cardiovascular system, immune system, and
mental health (in the areas of stress, depression, anxiety, and negative emotions). Evidence for the
effectiveness of forest-based interventions on metabolic parameters in adults, the severity of atopic
dermatitis in children and adolescents, and social skills and sociality in healthy primary school
children was weak. Discussion/Conclusions: Evidence suggests beneficial therapeutic effects of
forest-based interventions on hypertension, stress, and mental-health disorders, such as depression
and anxiety. Changes in immunological and inflammatory parameters after forest therapy should be
verified in bio-geographically native forests. In the future, more attention should be paid to careful
planning, implementation, and reporting of primary studies and to systematic reviews on the effects
of forest-based interventions.
Keywords: forest therapy; forest bathing; Shinrin-Yoku; forest medicine; prevention; systematic re-
views
Copyright: © 2021 by the authors.
Licensee MDPI, Basel, Switzerland.
This article is an open access article
distributed under the terms and
conditions of the Creative Commons
Attribution (CC BY) license (https://
creativecommons.org/licenses/by/
4.0/).
1. Introduction
Today, an increasing number of people worldwide live in urban rather than in rural
areas. This amounted to 55% of the world population in 2018, and the trend is rising [1].
While the world continues to urbanise, the value of natural environments, green spaces,
and forests for the quality of life and well-being of urban populations is becoming more
Int. J. Environ. Res. Public Health 2021, 18, 1770. https://doi.org/10.3390/ijerph18041770
https://www.mdpi.com/journal/ijerph

Int. J. Environ. Res. Public Health 2021, 18, 1770
2 of 38
and more evident. Exposure to nature and green environments is increasingly recognised
as an important resource for stress recovery and general health [2–5].
The Greater Tokyo Area is one of the world’s largest metropolitan regions with
about 37 million inhabitants [1]. It is, therefore, not surprising that the idea of forest
bathing originated in Japan. The Japanese Ministry of Agriculture, Forestry and Fisheries
introduced forest bathing (Japanese: “Shinrin-Yoku”) in the early 1980s and funded a
large research program to prove its medical and therapeutic effects [6]. The first centre for
“forest therapy” was later opened, and Japanese universities are now offering a medical
specialisation in “forest medicine”. In other Far Eastern countries, such as South Korea
and China, forest bathing is also a recognised form of both therapy and disease prevention
with a decades-long tradition. The concept of forest bathing has also arrived in the Western
world. The Scandinavian countries were among the first European countries to implement
projects on the healing effects of forests such as “Green Steps” in Sweden, “Power Trail at
Ikaalinen Spa” in Finland, and “Nacadia Therapy Forest Garden” in Denmark [7]. Healthy
people and those with pre-existing conditions participate in forest therapy programs of
various kinds for preventive and therapeutic purposes in the both the USA and Europe.
Forest bathing has become a global trend as a reaction to the current flood of stimuli and
the hectic daily life in our modern society [8,9].
The methods applied in forest therapy and prevention programs vary considerably. A
key component is the perception of the forest environment with all five senses (“five-sense
experience”, including vision, smell, hearing, touch, and taste), which can be combined
with meditation and walking or hiking in the forest, as well as various recreational activities
and cognitive behavioural therapy [10]. In Germany, forest therapy and forest bathing have
been successfully combined with classical naturopathic elements, such as water immersion
(e.g., Kneipp therapy) and climatotherapy (climatic terrain cure, heliotherapy, fresh-air
rest cure) to enhance the health benefits of forest therapy programs [11]. In 2017, the first
European “cure and healing forest” was established in Northern Germany in the seaside
resort of Heringsdorf on the Baltic Sea island of Usedom. The cure and healing forest
can be used both by patients from rehabilitation clinics and by the general population to
promote their own health and personal well-being, as well as for therapeutic interventions
in respiratory, cardiovascular, orthopaedic, and psychosomatic diseases [12]. Scientists
in German-speaking countries are also researching whether the native forest can be used
for preventive or medical purposes [13]. In 2017, the Forestry Faculty at the University of
Belgrade investigated a 30-hectare area at the Gocˇ Mountain in Serbia and proclaimed the
forest to be an appropriate “cure and healing forest”. This offers a new approach to health
tourism in Serbia [14].
Forest therapy and its presumed preventive effects have recently received growing
attention in the international scientific world. Many international studies have reported
the health-promoting effects of exposure to the forest environment on both body and
mind [9,11]. Primary studies, systematic reviews (SRs) and meta-analyses (MAs) have
been conducted to determine the preventive and therapeutic effects of forest bathing, forest
therapy, and forest medicine for various indications. Special attention has been paid to the
benefits of forest therapy on mental health, as especially people living in urban areas are at
increased risk of being exposed to stressful situations and developing chronic mental health
disorders [15–17]. As a result of sedentary and/or hectic lifestyles, chronic stress combined
with little physical activity plays an important role in the development of so-called diseases
of civilisation [18], such as chronic cardiovascular and respiratory diseases, diabetes, skin
diseases, and a weakened immune system [3,19]. Patients suffering from these types of
diseases are among the target groups of interventional studies in the forest environment.
Forest bathing is indicated not only for patients, but also for healthy individuals due to its
mainly preventive character. Improving the quality of life and increasing well-being are
particularly important goals.
The term “forest bathing” is derived from the Japanese “Shinrin-Yoku”, which literally
means “diving into the atmosphere of the forest”. Other terms frequently used in inter-
Int. J. Environ. Res. Public Health 2021, 18, 1770
3 of 38
national studies for interventions in forest environments are “forest therapy” and “forest
medicine”. Forest interventions are sometimes also called “forest (healing) programs”.
Schuh and Immich [11] proposed separate definitions for the two concepts “forest bathing”
and “forest therapy”. “Forest bathing” should be used for preventive purposes in healthy
people, while the term “forest therapy” should be used when interventions in the forest
are intended to achieve therapeutic goals in people with existing conditions. The authors
acknowledged that the two terms are not clearly separable in current usage. The term
“forest bathing” (Shinrin-Yoku) is common in the literature. In this paper, we generally use
“forest-based interventions” as a generic term for health interventions carried out in forests.
Nature therapy, nature-based rehabilitation, nature-based treatment programs, and
similar terms are also frequently used in the scientific literature when studying nature-based
therapeutic interventions [2,3,20]. As it is possible, but not mandatory, for nature-based
therapeutic interventions to include forest areas, we have only considered papers in our
systematic review on SRs and MAs that explicitly refer to forest-based interventions.
Our preliminary literature searches identified a large number of studies that could
be deemed suitable for inclusion in a systematic review on SRs and MAs. The literature
research by Meyer and Bürger-Arndt in 2014 [21] and the update which followed a few
years later [22] are among the most comprehensive literature surveys in this regard. Their
work, however, is a narrative review. Following a very comprehensive literature search,
the authors provided a narrative summary of the study results published up to that point.
Neither the effectiveness of the interventions nor the methodological quality of the reviews
was examined in greater detail.
We aimed to gain a comprehensive, up-to-date overview and an in-depth understand-
ing of which forest-based preventive and therapeutic interventions are effective for which
health conditions. The objective of our review was to synthesise evidence from SRs and
MAs that evaluated the effectiveness of forest-based interventions and to assess the quality
of the systematic reviews based on such studies.
2. Materials and Methods
A study protocol of this systematic review was registered with the International
Prospective Register of Systematic Reviews (PROSPERO), registration number
CRD42020190649 [23].
2.1. Literature Search
One author (V.T.) conducted a systematic literature search of 8 bibliographic databases
(MEDLINE, Embase, Web of Science, Cochrane Library, PsycInfo, CiNii, EBSCO, and
Scopus) from inception to the end of May 2020. A second author (M.K.) used Google
Scholar, PROSPERO, and the references of relevant reviews to search for related literature
that may have been overlooked. All search terms are listed in Appendix A. There were no
restrictions regarding the publication language.
2.2. Inclusion and Exclusion Criteria
We generally aimed to identify all systematic reviews with or without meta-analyses
that systematically searched for the effects of forest bathing (Shinrin-Yoku), forest therapy,
or forest medicine of any kind, and summarised and reported them. The inclusion and ex-
clusion criteria were based on the PICOS (Population, Intervention, Comparator, Outcome,
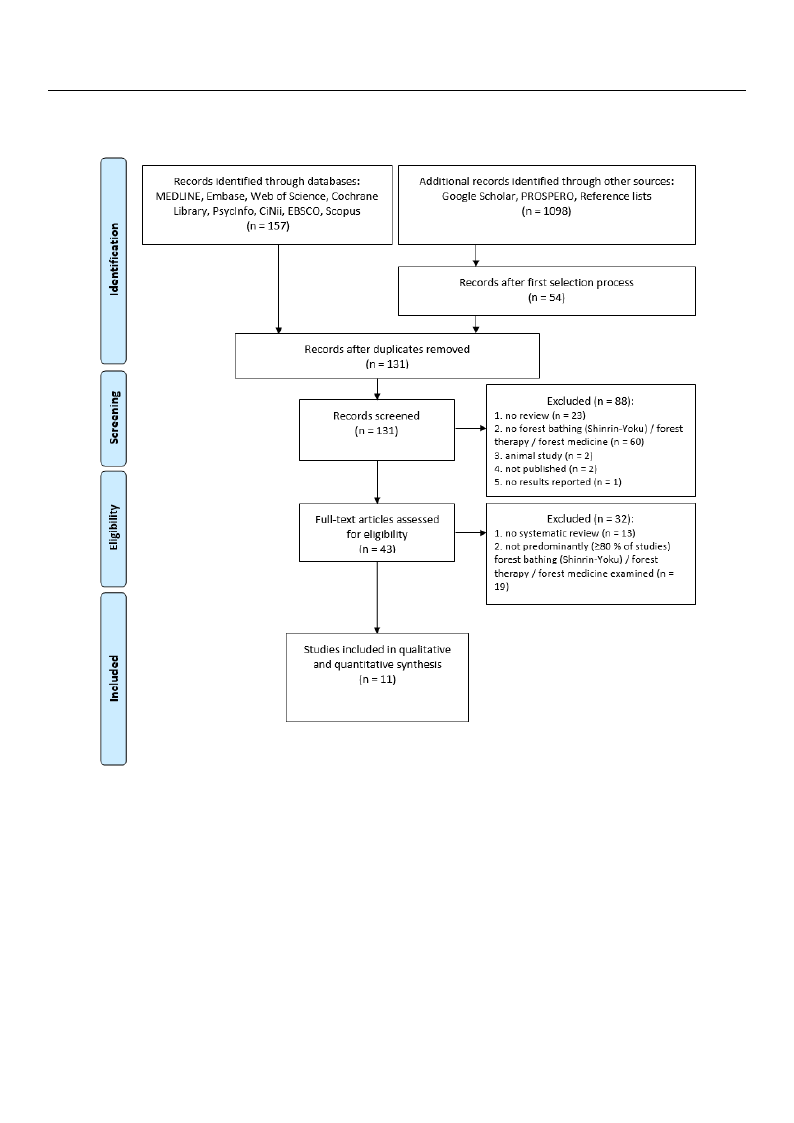
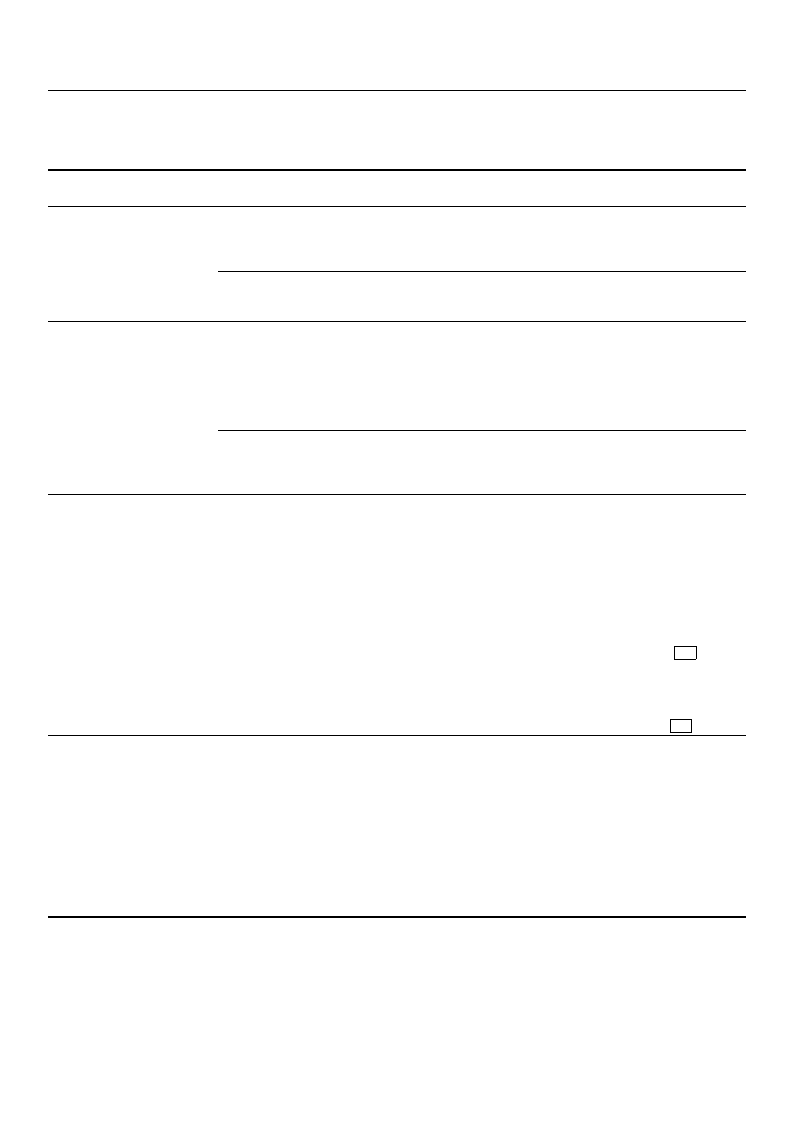
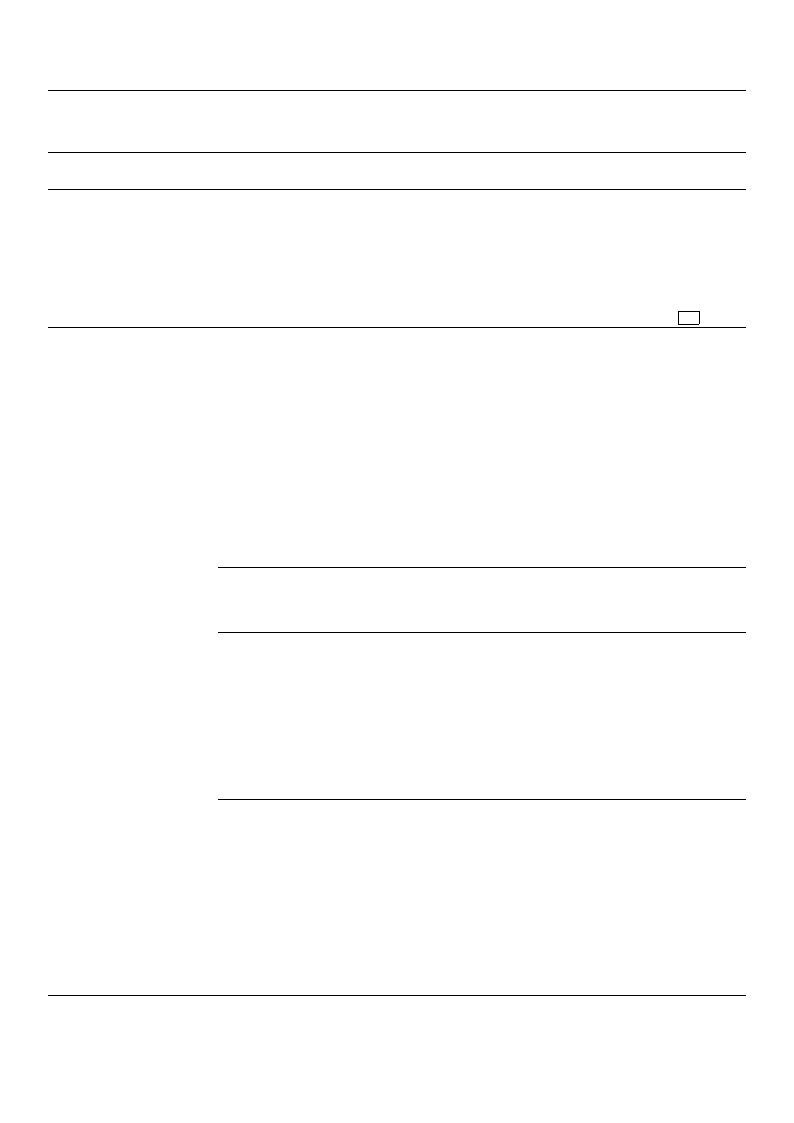
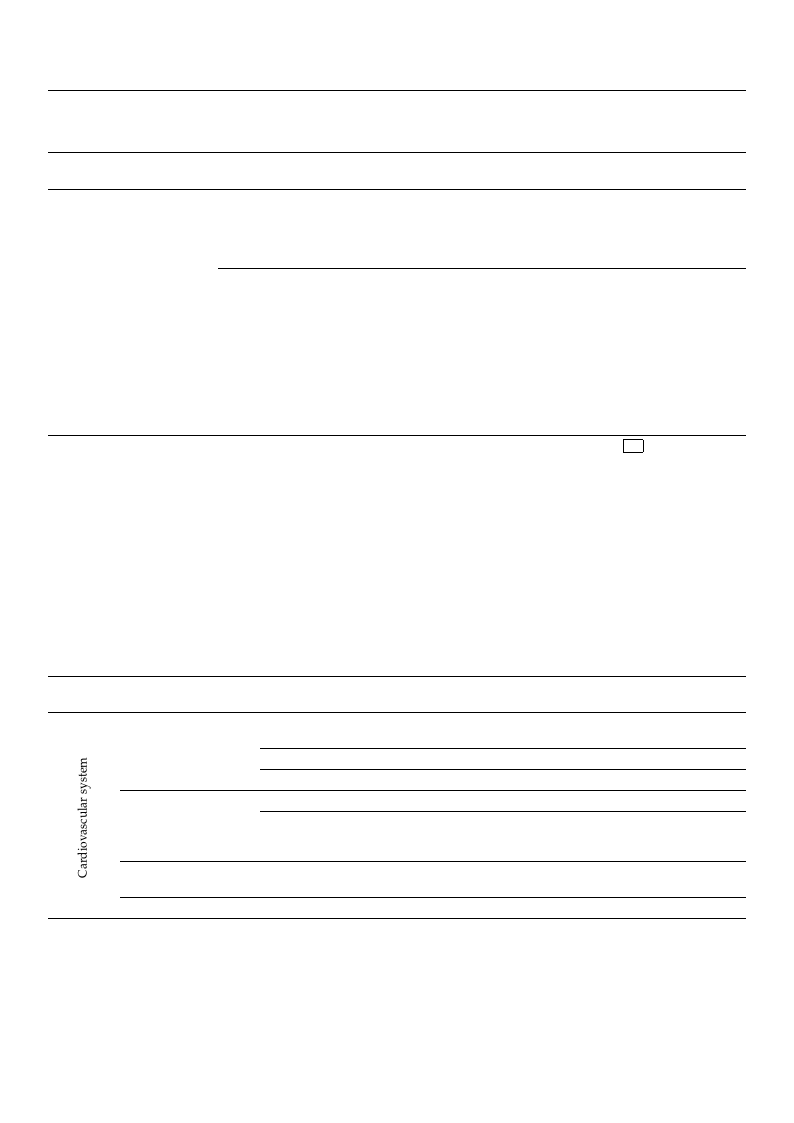
Study design) elements [24] (Figure 1).
SRs and MAs on randomised (RCT) or non-randomised controlled trials (NRCT) and
non-controlled trials (NCT) were eligible if they had used at least 2 databases for their
literature search and at least 80% of the studies included had investigated forest-based
interventions.
We excluded reviews (1) with a different study design than defined in inclusion
criteria (e.g., narrative review), (2) where more than 20% of the primary studies contained

interventions that were not carried out in forests (e.g., nature, park, field), and (3) that
included theoretical studies or published opinions as their primary sources of evidence.
2.3. Deviation from the Study Protocol
Int. J. Environ. Res. Public Health 2021, 18, 17T70here were two changes made to the study protocol: (1) We originally plann4edof t3o8
exclude reviews where the study selection and/or data extraction had not been performed
independently by two reviewers. This criterion was not applied in the review-selection
process. (2) According to the protocol, only reviews containing exclusively forest-based
sintutedriveesnwtieornestothbaet iwncelruedneodt. Icnasrtreieadd,oruevt iienwfsorwesetrse (ien.cgl.u, dneadtuirfea,tpleaarskt, 8fi0e%ldo),f athnedp(r3i)mtharayt
sintuclduidesedintchlueodreedticwaelrsetufodrieessto-brapsuedbl.ished opinions as their primary sources of evidence.
Figure 1. Inclusion and exFcilguusrioen1.cIrnitcelruisaiobnasaenddoenxcPluICsiOonS c(rPitoepriualabtaiosend, IonntePrIvCeOntSio(nP,opCuolmatpioanra, tIonrt,erOvuentctoiomne, ,CSotmudpyarator,
design) [24].
Outcome, Study design) [24].
2.43. SDeelevcitaitoinonofrSotmudthieesStudy Protocol
AThfteerreawn einreititawl soelcehcatinognebsamseaddoentothtehelisgtuibdilyityprcorittoecroial:a(n1d) W the roermigoinvalloyfpdluapnlniceadtetso,
wexecleuxdaemreinveiedwtshwe htietlreesthanedstuabdsytrsaecletsctoiofnthaendid/eonrtdifaietadesxtturadciteisonfohratdheniortrbeelevnapnecref.oIrfmtehde
infdoerpmeantdioenntilnytbhye twitloe arenvdieawbsetrrsa.cTt hwiasscrinitseurfiofinciewnats, tnhoetfaupllptleixetdwinasthaenarelyvsiedw(-fsoerleicntfiorn-
mpraotcieosns.on(2e)xAclcucdoreddinregfetroetnhceespirnottohcisosl,teopn,lysereeAvipepwesncdoixntBa)i.nAinbgsterxaccltuasnivdefluyllf-oterexstts-cbraeseend-
isntugd, iseeslewcteiroentopbroecienscsl,uddaedta. Ienxsttreaacdti,orne,viaenwds qwuearleitiyncalsusdeesdsmifeanttlewaesrte80c%arroifetdheouptriminadrey-
psteunddieens tilnyclbuyde3dawutehroerfsor(eVs.tT-b.,aMse.dK.., M.S.J.). Each reference was reviewed by 2 of the 3
authors. Discrepancies were clarified through discussion with the involvement of the
t2h.4ir.dSealuectthioonr.oIfnStthuediqesuality assessment, the interrater reliability was calculated using Co-
hen’sAkfateprpaan. initial selection based on the eligibility criteria and the removal of duplicates,
we examined the titles and abstracts of the identified studies for their relevance. If the
2in.5fo. rQmuaatliiotynAinsstehsesmtietlnetand abstract was insufficient, the full text was analysed (for informa-
2iottcstbneiherfyo(mesleAneatp3rqacaouMTttatunioinmuhocatcentleaeiraeihelxetnsmpoysvcuotrrlwierafou(seteAscwdhe1(mseVrM6eoesseed.sdsTqoSnsc,o.rmuTflt,delareoAMTfareasegitonRntfira.iioKtecd-oe,el2na.dnotx,)tlchmsotMeqcterhosuAwai.isrmcSianoesint.ltstduipJiheoett.gr)yhrasn.irshsins,oaiEsemdSadtfassenyiitcpnr1snsdehocl0trpceeueqnlr,romulseu-sifrsdfaaeaaaeitnbeelohtnriidisneteAcldwyinStowoRpycaeRmrpeersiiwstvgseihwoesinaiaenpesntadswsdhatsdimiclexsocraM1)eeoniBl1ncenvns)Auxvt.iete(plrosAxw“awolliwYtbivsleeceltseereadiidtetmsndsrl”uygacbae,cacsysncldt“irisrntnriN2aeimigtoinseoicofscdedCaf”eatnl,odtholfsthluhue“ryiueolieptltasann-h3ailitpnss’nrieasr.ptdxgadiuTkraetnAtahaplasdhipecueMsYorcpnitrreenohSedassegnoTv..e”nsriAnDs)i.si.yntseRIilAstgsndys---,
c2o.5m. QprueahlietnysAivsesegssumidenetis available for users [25].
The methodological quality of included SRs and MAs was assessed using AMSTAR-2
(A Measurement Tool to Assess Systematic Reviews) explicitly critically appraising sys-
tematic reviews of randomised and non-randomised controlled clinical trials. The revised
instrument (AMSTAR-2) comprises 10 of the original 11 existing dimensions and consists
of a total of 16 questions with simpler answer options (“Yes”, “No”, “partial Yes”). A
comprehensive guide is available for users [25].
On the basis of 7 so-called critical domains (items 2, 4, 7, 9, 11, 13, and 15) which can
decisively influence the validity of a review and its conclusions, we made an assessment for
each included review as to whether the confidence in the results of the review could be rated
“high”, “moderate”, “low”, or even “critically low” [25,26]. The authors of the Guidance
Document explicitly offer AMSTAR-2 users the option to deviate from the Guideline, if
necessary. Appendix C gives a detailed description of the adjustments for the quality
assessment of the current SRs and MAs.

Int. J. Environ. Res. Public Health 2021, 18, 1770
5 of 38
2.6. Data Extraction
The following information on the SRs and MAs was extracted from the full texts of
the relevant publications: reference, study objective/question, type of review, number
of included primary studies, number and names of databases searched, search period,
quality assessment tool(s) for included studies, results of the quality assessment (internal
validity, quality of evidence), conflicts of interest, method of synthesis/analysis, and main
results. We also extracted information on the studies included in the SRs and MAs: study
design, publication period of the included primary studies, study populations, number of
participants, interventions, countries/regions where the interventions were carried out,
control/comparison groups and their interventions, duration of follow-up, indications,
outcomes, and results.
3. Results
3.1. Search Results
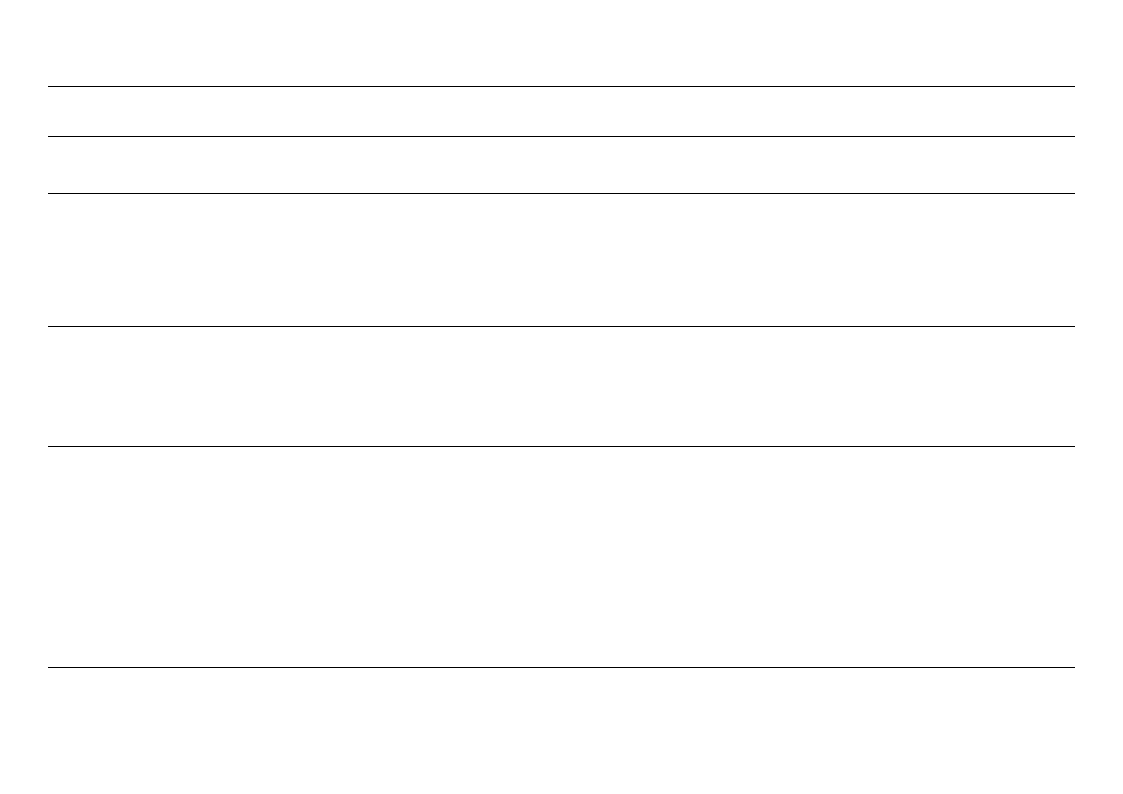
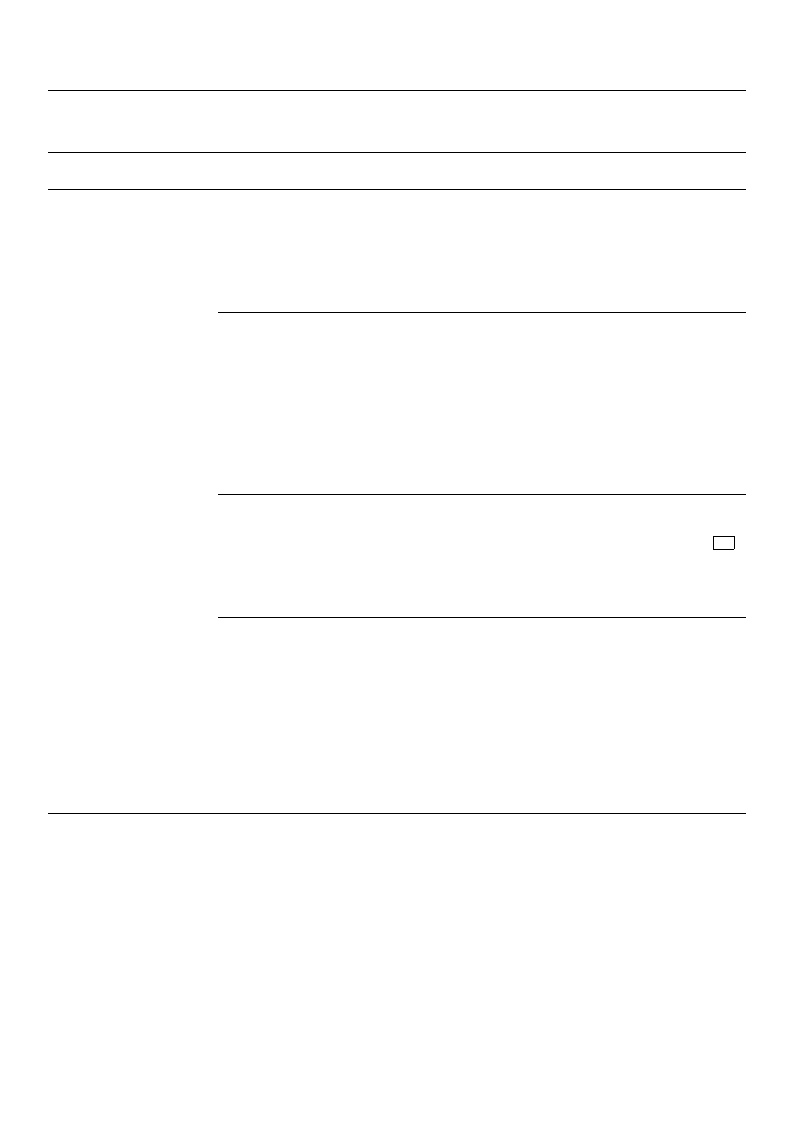
The search identified 131 potentially relevant abstracts. After abstract screening,
88 records were excluded. The remaining 43 full-text articles were assessed for eligibility.
Eleven SRs and MAs were finally considered eligible (Figure 2). All excluded articles are
listed in Appendix B.
3.2. Characteristics of Included Studies
The characteristics of the included SRs and MAs, including key details of the covered
primary studies, are presented in Table 1.
The SRs and MAs were published between 2016 and 2019. Four of these were con-
ducted in Korea and one each in Japan, Australia, Indonesia, Italy, the USA, China, and the
UK. Three included papers were systematic reviews with additional meta-analyses [27–29].
Most of the reviews examined the effects of forest-based interventions for specific indi-
cations, such as stress or depression [27,29–34]. Three studies are broader in scope and
examined the health effects of forest-based interventions without focusing on specific con-
ditions [19,35,36]. In five reviews, both study selection and data extraction were performed
independently by two reviewers [19,27,32–34]. In four other reviews, either study selec-
tion [29,31] or data extraction [28,36] was performed by two reviewers, and in two reviews,
neither was performed by two reviewers [30,35]. The authors of seven reviews stated
that there were no conflicts of interest [19,28,30,32,34–36]. Four others did not provide
conflict-of-interest statements [27,29,31,33]; one reported that no financial support was
received for the preparation of the paper [29].
The 11 included SRs and MAs cover a total of 131 individual studies that examined
the health effects of forest-based interventions. The studies were published between 1996
and 2019, with a particularly high proportion of publications in the years 2013 to 2015.
Thirty-nine primary studies were RCTs, 55 NRCTs, and 32 NCTs. No information on the
designs was available for a further five studies that were included exclusively in Putra’s
systematic review [33].
More than three quarters (75.6%; N = 99) of individual studies were included in only
1 of the 11 reviews, 16.0% (N = 21) were included in two reviews, 6.1% (N = 8) in three
reviews, one study was included in four, and two studies were included in five reviews.
Int. J. Environ. Res. Public Health 2021, 18, 1770
6 of 38
First Author
(Date);
Country
Lee (2016);
South Korea [31]
Ideno (2017);
Japan
[28]
Lee (2017);
South Korea
[32]
Table 1. Characteristics of included reviews and meta-analyses including key details of the covered primary studies.
Search Details
Objective;
Meta-Analysis: Yes/No
Assessment of Risk of Bias and/or
Study Quality:
6 DBs, from inception
to Nov. 2015;
GL: unpublished
dissertations
considered
Effects of forest
programs on atopic
dermatitis;
LR: n. a.
No
RoBANS
SB: confounder and selection of
participants—high,
comparability—predominantly low
PB: high
DB: high
AB: predominantly low
RB: predominantly low
4 DBs, from inception
to May 2016;
GL: was searched
LR: English and
Japanese language
only
Effects of the forest
environment on blood
pressure;
Yes
RoB
SB: high (with 50%)
PB: high
DB: high
AB: low
RB: low
7 DBs, from inception
to July 2016;
GL: n. a.
LR: English and
Korean language only
Effects of forest therapy
on depressive
symptoms;
No
SIGN checklist
18 studies low and
10 acceptable quality
Number (Type) of Studies
Included;
Country of Study
Implementation
N = 5 (5 NCT);
Korea
Study Population;
Total Number (Range)
Children, adolescents with
atopic dermatitis;
184 (12–64)
Interventions: Intervention Group
(IG) and Control Group (CG);
Intervention Duration
IG: forest experience, forest trip;
forest camp; physical therapy;
forest-camp swimming; forest
activities, disease education
CG: n. a.;
Durations: 1–3 days (3–4 nights)
N = 20 (2 RCT, 15 NRCT
cross-over, 3 NRCT);
Japan (n = 17)
Korea (n = 2)
China (n = 1)
N = 28 (17 RCT,
11 NRCT);
Korea (n = 17)
Japan (n = 7)
China (n = 3)
Great Britain (n = 1)
Healthy adults, adults with
hypertension;
732 (6–268)
Healthy adults, adults with
health conditions:
alcoholism, COPD, chronic
stroke, hypertension, cancer,
mental-health conditions,
psychiatric out- and
inpatients, major depression
disorder;
1090 (11–92)
IG: walking in/sitting in and
viewing forest area
CG: walking in/sitting in and
viewing in non-forest environment,
such as city areas, sitting in a room,
measuring blood pressure in daily
life;
Durations: 15 min to 2 h; 1 × 3 days,
1 × 7 days
IG: forest therapy: walking as a key
component in the forest, other
therapeutic activities (experiencing
the forest through all five senses:
seeing, hearing, touching, smelling,
tasting), viewing the
forest/meditation, Qi-Qong,
aromatherapy, herbal tea therapy,
handicrafts with natural items
CG: normal daily routine; conducted
same activities in the room/city
area/urban forest/hospital/stay in
a hotel; regular diet and exercise
program in the forest; one-day trip
for urban walking;
Durations: 12 min to 3 days for 1
day to 12 weeks
Int. J. Environ. Res. Public Health 2021, 18, 1770
7 of 38
First Author
(Date);
Country
Oh (2017);
Australia
[19]
Song (2017);
South Korea
[34]
Chae (2018);
South Korea
[35]
Table 1. Cont.
Search Details
Objective;
Meta-Analysis: Yes/No
Assessment of Risk of Bias and/or
Study Quality:
5 DBs, from inception
to Dec. 2016;
GL: was searched
LR: English language
only
Effects of forest bathing
on health;
No
RoB
SB: high (with 66%)
PB: high
DB: high (with 30%)
AB: unclear or low
RB: low
6 DBs, from inception
to Dec. 2016;
GL: n. a.
LR: English and
Korean language only
Effects of forest therapy
programs for
elementary-school
students;
No
RoBANS
SB: confounder high (with 50%);
comparability—predominantly low;
selection of participants—low
PB: high
DB: high
AB: predominantly low
RB: predominantly low
5 DBs, from inception
to March 2018;
Effects of forest healing
GL: n. a.
therapy;
n. a.
LR: English and
No
Korean language only
Number (Type) of Studies
Included;
Country of Study
Implementation
N = 6 (6 RCT);
China (n = 3)
Korea (n = 2)
Sweden (n = 1)
N = 17
(two of them without forest
intervention;
10 NRCT,
7 NCT);
South Korea
N = 25
(5 of them without forest
intervention; 13 NRCT,
12 NCT;
Korea
Study Population;
Total Number (Range)
Healthy adults, adults with
health conditions: chronic
alcoholic, high blood
pressure, exhaustion
disorders, COPD;
323 (18–99)
Healthy children;
1491 (16–308)
Nurses, healthcare worker,
healthy adults, adults with
health conditions:
alcoholism,
Hwa-Byung, depression,
mild cognitive impairment,
cancer;
1141 (10–221)
Interventions: Intervention Group
(IG) and Control Group (CG);
Intervention Duration
IG: forest-healing camp (interaction
with nature; mountain climbing und
trekking; self-introspection,
including mediation and
counselling); mountain-forest walks;
forest-rehabilitation group (with
subsequent cognitive behavioural
rehabilitation for all participants)
CG: normal daily routine;
walking/hiking/interventions in
urban area/city; waiting list group
with cognitive behavioural
rehabilitation;
Durations: 1h to 2× week for 11
weeks (22 visits each with 4 h)
IG: walks; forest athletic meetings;
getting along with neighbours;
forest-ecology exploration; making
something with natural materials;
psychotherapy; climate therapy;
exercise therapy; diet therapy; water
therapy
CG: normal daily routine;
traditional learning methods,
reduced forest program at school;
Durations: 5 h to 8 months
IG: nature-experiencing physical
activities; forest (healing) program;
meditation; hiking
CG: interventions conducted
indoors; other settings (ambulatory
treatment); comparator duration of
intervention; no intervention;
Durations: 1 day to 12 weeks
Int. J. Environ. Res. Public Health 2021, 18, 1770
8 of 38
First Author
(Date);
Country
Putra (2018);
Indonesia[33]
Antonelli, (2019);
Italy[27]
Farrow (2019);
USA
[30]
Table 1. Cont.
Search Details
Objective;
Meta-Analysis: Yes/No
Assessment of Risk of Bias and/or
Study Quality:
2 DBs, from 2007 to
July 2017;
Effects of phytoncides
GL: n. a.
when forest bathing;
n. a.
LR: English language No
only
6 DBs, from inception
to Feb. 2019;GL: was
searched
LR: English, French,
Spanish, and Italian
only
Effects of forest bathing
on levels of salivary or
serum cortisol as stress
biomarkers;
Yes
NIH; RoB
SB: low or unclear
PB: high
DB: low
AB: low or unclear
RB: low
2 DBs, from 2008 to
2018;
GL: n. a.
LR: n. a.
Effects of forest bathing
on reducing anxiety
and heart rate
variability (activation of n. a.
parasympathetic
nervous system);
No
Number (Type) of Studies
Included;
Country of Study
Implementation
N = 10 (n. a.);
Japan
N = 22 (3 RCT, 8 RCT
cross-over, 5 NRCT,
3 NRCT cross-over,3
NCT);Japan (n = 12)
South Korea (n = 4)China (n
= 2)
Germany
(n = 1)
Iceland (n = 1),
Finland (n = 1)
Spain (n = 1)
N = 10 (2 RCT, 3 RCT
cross-over, 1 NRCT
cross-over, 1 NRCT,
3 NCT);
Japan (n = 8)
Taiwan (n = 1)
Finland (n = 1)
Study Population;
Total Number (Range)
Healthy adults;
126 (12–17)
Healthy children and adults,
adults with health
conditions: COPD, high risk
of stress/burnout, major
depressive disorder,
hypertension,
post-menopausal women;
2165 (9–348)
Healthy adults,
hypertensive adults;
1667 (9–625)
Interventions: Intervention Group
(IG) and Control Group (CG);
Intervention Duration
IG: walking, sitting and watching in
the forest; physical activity; stay in
the hotel for 3 days and 3 nights and
giving aromatic volatile substances
(phytoncides produced by
vaporising Chamaecyparis obtusa
stem oil) with a humidifier in the
hotel room for 3 nights
CG: city trips: walking, sitting and
watching; normal physical activity;
Durations: 4.5 h to 2–3 days
IG: forest bathing: spending time in
a forest, walking, resting, watching,
and deep breathing in forest;
psychological program; cognitive
behaviour therapy
CG: walking and/or watching an
urban area/-park; spending time on
beach; no intervention; indoor;
psychological program; comparator
age;
Durations: 15 min to half a day
IG: walking, sitting in forest
environment, viewing a forest
landscape
CG: walking, sitting in urban
environment, viewing an urban
landscape;
Durations: 15 min half a day
(4–4.5 h); 15 min on 2 days in a row
Int. J. Environ. Res. Public Health 2021, 18, 1770
9 of 38
Table 1. Cont.
First Author
(Date);
Country
Search Details
Objective;
Meta-Analysis: Yes/No
Assessment of Risk of Bias and/or
Study Quality:
Number (Type) of Studies
Included;
Country of Study
Implementation
Study Population;
Total Number (Range)
Interventions: Intervention Group
(IG) and Control Group (CG);
Intervention Duration
Wen (2019);
China
[36]
3 DBs from 2015 to
April 2019;
GL: was searched
LR: English language
only
Effects of forest
environment exposure
on human health;
No
Downs and Black Checklist
16 studies high- and 12 studies
low-quality;
RoB relatively high overall
N = 28 (7 RCT,
10 RCT cross-over,
1 NRCT cross-over,3 NRCT,
7 NCT);
Japan (n = 13)
China (n = 6)
South Korea (n = 5)
Taiwan (n = 3)
Poland (n = 1)
Healthy children, adults,
adults with health
conditions: high blood
pressure, COPD, chronic
stroke, chronic heart failure;
924 (6–128)
IG: exposed to forest (urban forest
park), walking, meditation, “five
sense experience”, activities and rest,
watching the scenery—forest
environment, handicrafts, sitting
quietly in a dense/sparse forest
environment; taking a
tree-measuring course; enjoying
private time
CG: exposed to urban
environment/walking and
meditating; watching the
scenery—urban environment; sitting
quietly in a dense/sparse forest
environment; indoor classes;
Durations: 15 min to 5 days
Kotera (2020);
United Kingdom
[29]
4 DBs from inception
to Oct. 2019;
GL: was searched
LR: English language
only
Effects of Shinrin-Yoku
(forest bathing) and
nature therapy on
mental health;
Yes
1. NOS
2. Quality Assessment Table of
Randomised Controlled Trials
RCTs high to medium; RoB in 6
studies low and in 2 studies high
N = 20 (11 RCT, 2 NRCT,
7 NCT);
Japan (n = 10)
Korea (n = 4)
Taiwan (n = 2)
Poland (n = 2)
China (n = 1)
Serbia (n = 1)
Healthy adults, adults with
health conditons: metabolic
syndrome, chronic stroke,
psychiatric disorders
(depression), chronic
diseases, chronic pain,
alcoholism;
2257 (12–585)
IG: Walk in forest and meditation
CG: Crossover (forest vs. city);
groups with different forest types
(birch, maple, and oak);
Durations: 15 min to 9 days
AB: attrition bias; CG: control group; COPD: chronic obstructive pulmonary disease; DB: detection bias; DBs: databases; GL: grey literature; IG: intervention group; LR: language restriction; MA: meta-analysis; n.
a.: not applicable or not specified; NCT: uncontrolled trial; NIH: National Institutes of Health; NOS: Newcastle–Ottawa Scale; NRCT: non-randomised controlled trial; PB: performance bias; POMS: Profile of
Mood States; RB: reporting bias; RCT: randomised controlled trial; RoB: Cochrane Risk-of-Bias tool for randomised controlled trials; RoBANS: Cochrane Risk of Bias Assessment tool for Non-randomised Studies;
SB: selection bias; SIGN: The Scottish Intercollegiate Guideline Network measurement tool; SR: systematic review.
Int. J. Environ. Res. Public Health 2021, 18, 1770
Int. J. Environ. Res. Public Health 2021, 18, 1770
10 of 38
6 of 43
Figure 2. PRISMA (PreferredFiRgeupreor2ti.nPgRIItSeMmsAfo(Pr rSeyfsetrermedatRicepRoervtiienwgsItaenmdsMfoertaS-Aysntaelmysaetisc) flRoewviecwhasrtanfodr Mtheetsae-lAecntaiolynseosf) flow
reviews [37].
chart for the selection of reviews [37].
TThheen1u1minbcelur doef dstSuRdsieasnidncMluAdesdcoinvetrhea rteovtaiel wofs1v3a1riienddibveitdwueaelnst5ud[3i1e]s athnadt2e8xa[3m2i,3n6e]d.
Tthheerheewalaths aefcfoenctssidoefrfaobrleesvt-abraiasetidoninitnertvoteanltsioanmsp. lTehseizsetsu,driaensgwinegrefrpoumbl1i2sh6e[d33b]ettow2e2e5n7 1[2999]6
paanrdtic2i0p1a9n,tsw. iTthheasptuadrtyicpuolaprulylathioignhs ipnrcolupdoretdiohneaolfthpyucbhliicldatrieonn,sadinoltehseceynetasr, san2d01/3ortoad2u0l1t5s.
aTnhdirptyeo-npilneewpirthimhaeraylthstcuodniedsitwioenrseaRndCTdsis,e5a5seNs.RMCTost, aonf tdh3e2stNudCiTes.wNeoreincofonrdmucateiodninonAsthiae
(dSeosuigthnsKworaesa,aJvaapilaanb,lCe hfoinr aa, faunrdthTeariwfivaen)s,tuanddiefsetwhaetr wineEreurinocpleud(Peodlaenxdcl,uSspivaeinly, GinerPmuatrnay’s,
Iscyeslatenmd,aFtiicnrlaenvide,wSe[r3b3i]a., Great Britain, and Sweden) (Table 1).
More than three quarters (75.6%; N = 99) of individual studies were included in only
31.3o.fMtheeth1od1orloegviiceawl Qs,u1a6li.0ty%of(NInc=lu2d1e)dwReevreiewinscluded in two reviews, 6.1% (N = 8) in three
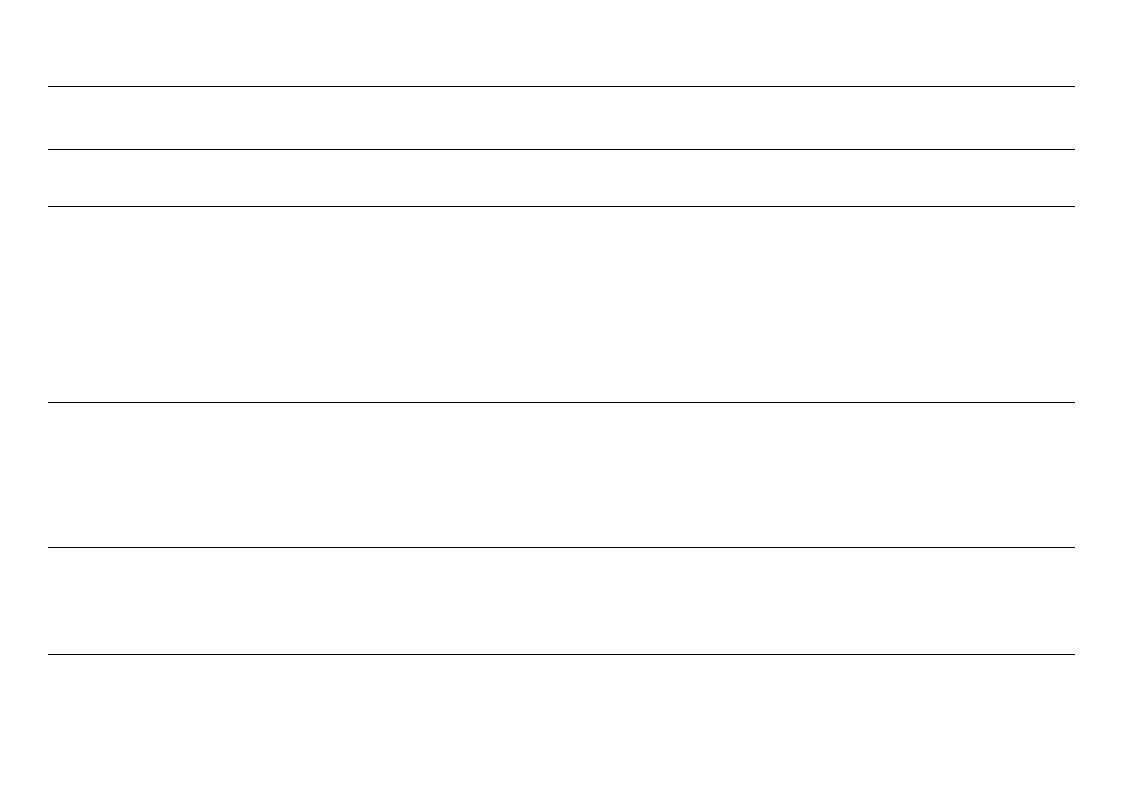
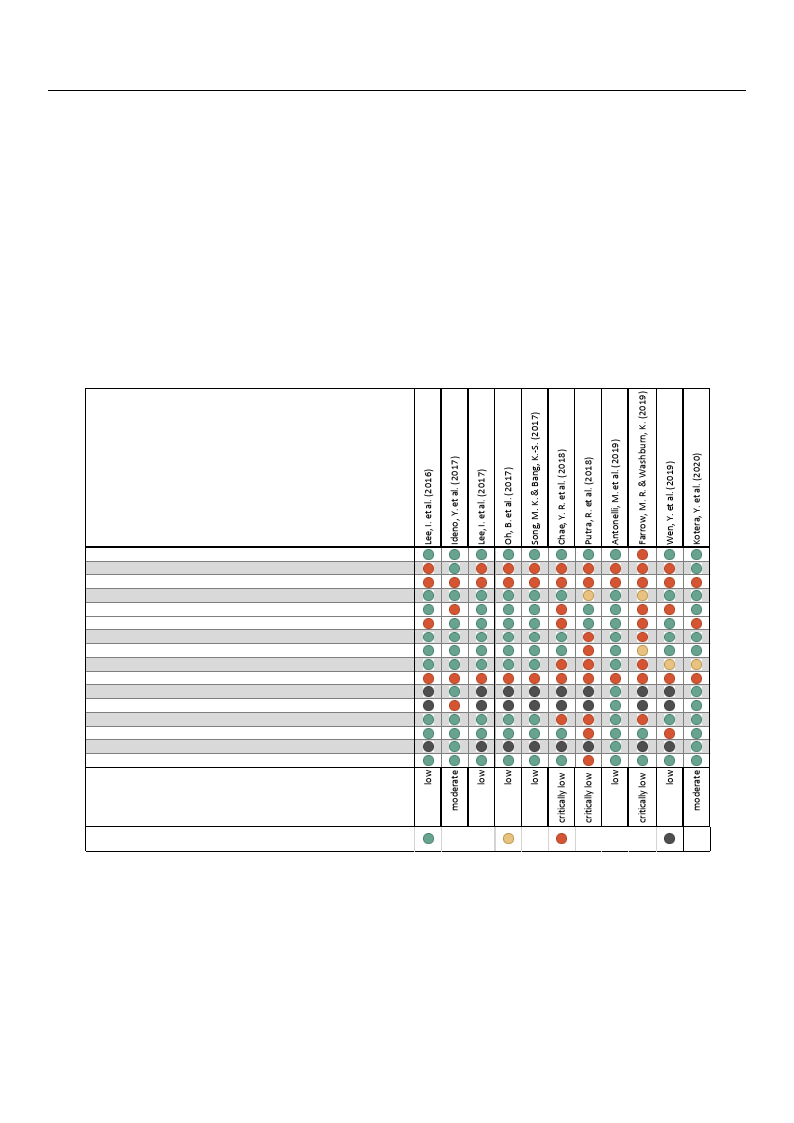
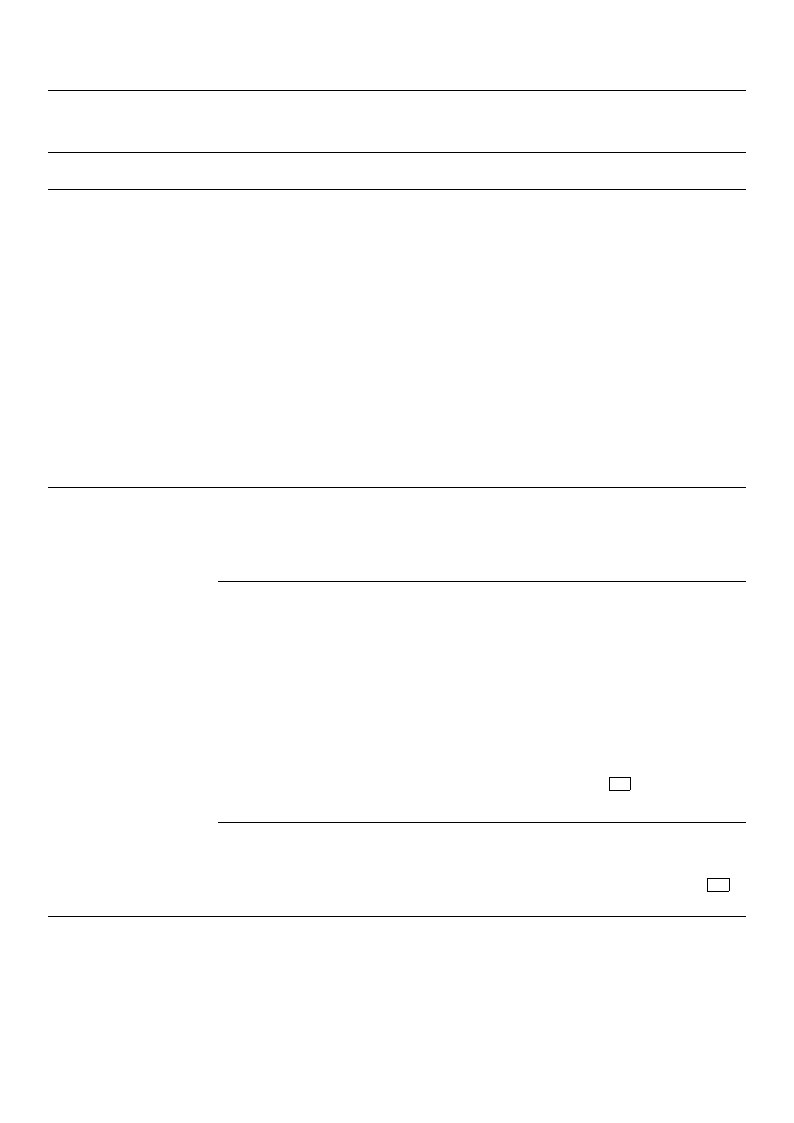
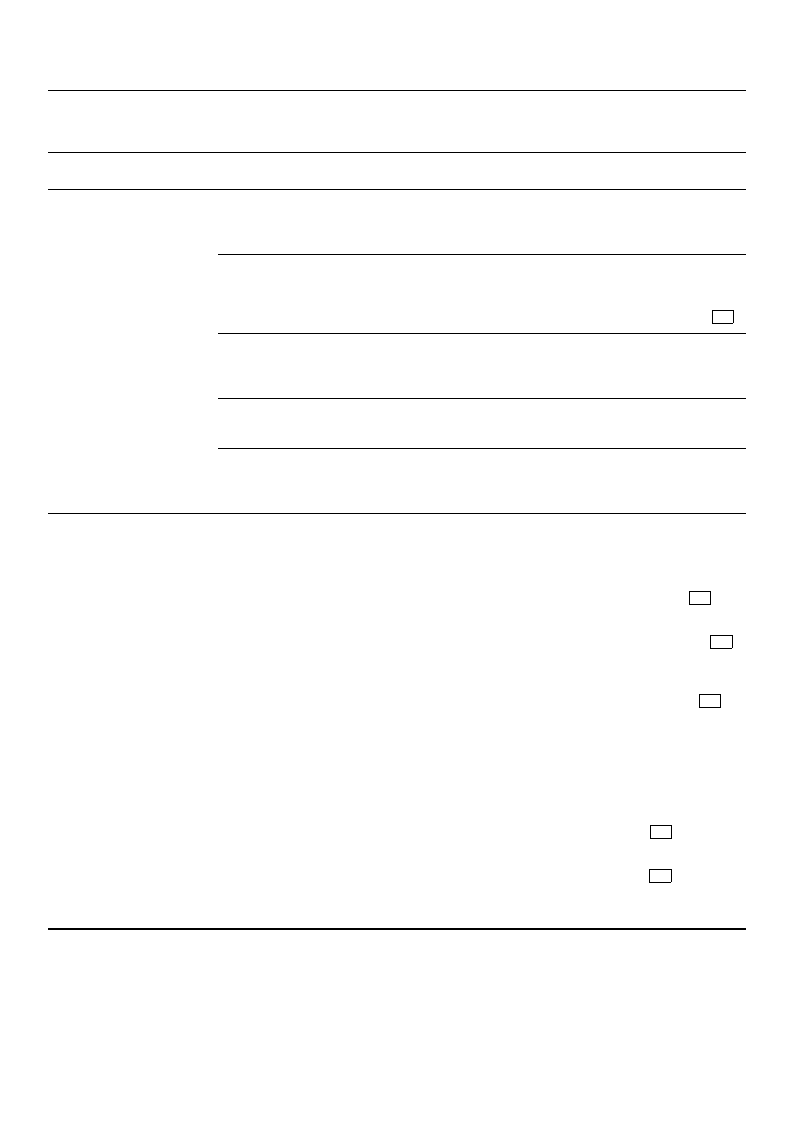
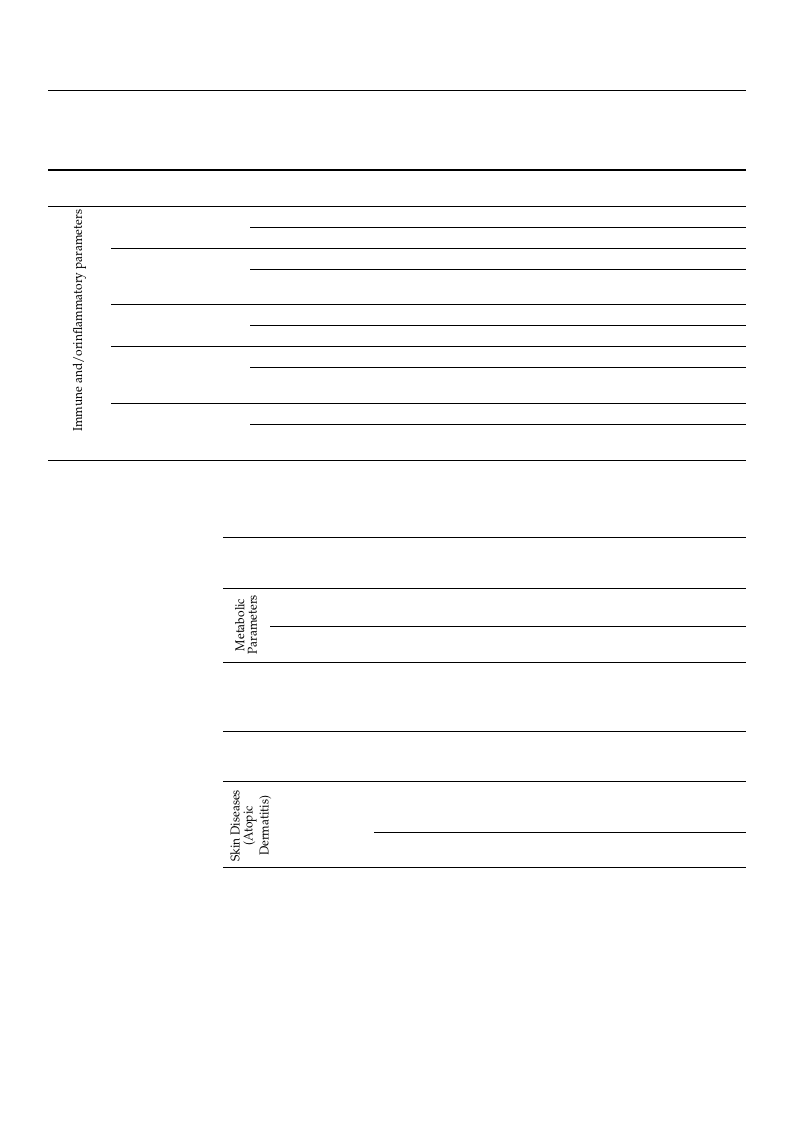
revieFwigsu, roen3epsrtuovdiydewsaassiunmclumdaerdy oinf tfhoeurA, ManSdTAtwRo-2srtuesduiletss.wTehreecionnclfiuddeendceinlefvivelesrienvtiheewrse.-
sults oTfhtehenuremvbieewr sofwsetruedfioeusnindctloudbedmiondtehreatreevinietwsov[2a8ri,2e9d],bleotwweinensi5x [3119],2a7n,3d1,2382,[3342,,3366]],.
aTnhderceriwticaaslalycloonwsidinerthabrele v[3a0r,i3a3ti,o3n5]i.nCtontaslesnasmuspelestsiimzeast,ersaonfgiinntgerfraotmer1r2e6li[a3b3i]litoy 2s2h5o7w[e2d9]
gpoaordticriepsaunlts.(Tpehrecestnutdagyepaogprueelamtieonnts8i4n.c7l%udaenddhCeoahltehnysc’ hki=ld0r.e7n7,).adNoolnesecoefnths,earnedv/ioewr asdmueltts
and people with health conditions and diseases. Most of the studies were conducted in
Int. J. Environ. Res. Public Health 2021, 18, 1770
11 of 38
the criteria covered by AMSTAR-2 Item 3 (explanation of the selection of study designs for
inclusion) and Item 10 (reporting sources of funding for studies included in the review).
However, both domains are not considered critical in the sense of the AMSTAR-2 defini-
tions. The failure to take these two points into account, together with the study selection
and/or data extraction not being carried out independently by two authors, resulted in
two reviews being rated with moderate rather than high confidence [28,29]. The main
reason for judging six reviews to be of low quality according to the AMSTAR-2 guidelines
was the lack of a study protocol, which should have been registered, published, or at least
prepared prior to starting work on the review. A study protocol is also missing in the
reviews that were assessed as critically low [30,33,35]. The latter left at least two other
nt. J. Environ. Res. Public Health 2021, 18, 1770
critical domains unconsidered: the application of a satisfactory technique for assessing the 17 of 4
risk of bias (RoB) in individual studies included in the review and consideration of the
RoB in the interpretation of the review results. Two of the reviews rated with critically low
and/or inflammcaotniofindpeanrcaemdetiedrsn, oant dreopthoerrt ltahbeorraetaosroynvsalfuoers)t.hPeateixencltu-rseiloevnaonft esntuddpoieins.ts are only found in the studies on ski
diseases (atopic dermatitis) and mental health.
Author
Item 1: Research questions and inclusion critria indluded PICO
Item 2: Protocol registered before commencement of the review
Item 3: Explanation of the selection of study designs for inclusion
Item 4: Adequacy of the literature search
Item 5: Study selection performed in duplicate
Item 6: Data extraction performed in duplicate
Item 7: Justification for excluding studies
Item 8: Studies included described in adequate detail
Item 9: ROB from individual studies being included in the review
Item 10: Reporting sources of funding for studies included in the review
Item 11: Appropriateness of meta-analytical methods
Item 12: Assessment of potential impact of ROB on results
Item 13: Consideration of ROB when interpreting the results of the review
Item 14: Heterogeniety satisfactorily explained and discussed
Item 15: Assessment of presence and likely impact of pulication bias
Item 16: Reporting of potential conflicts of interest and review funding
Confidence in the results of the review
Yes:
Partial Yes:
No:
No Meta-Analysis:
Figure 3. Quality assessment of included reviews based on AMSTAR-2. Critical domains are highlighted in grey. RoB: risk
of bias.
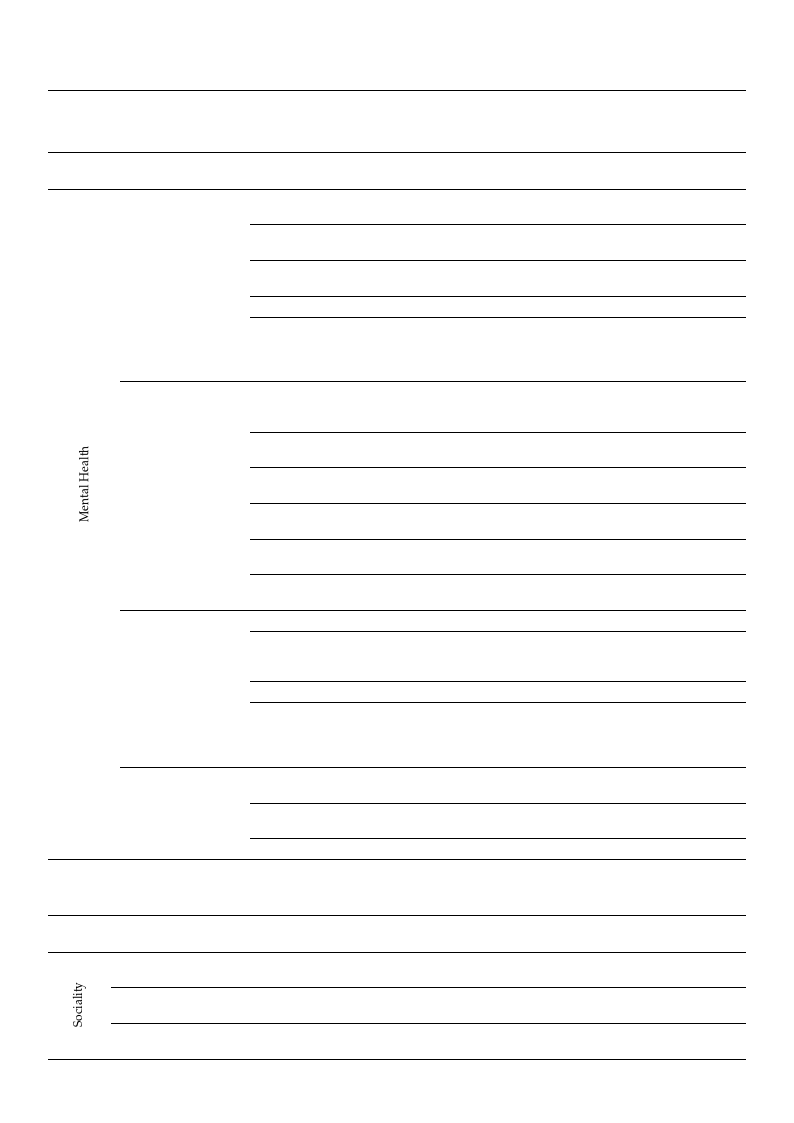
3.4. Summary of Main Findings
Tables 2–8 summarise the main findings for the included SRs and MAs. The three
reviews in which the quality assessment based on AMSTAR-2 (Figure 3) had shown
critically-low confidence in the results were not considered in Tables 3–8.
Int. J. Environ. Res. Public Health 2021, 18, 1770
12 of 38
Table 2. Summary of included reviews and meta-analyses—study populations, indications, and results of the included
primary studies, arranged in descending order by methodological quality.
Author
AMSTAR-2
Rating
Ideno, Y. et al.
(2017)
moderate
[28]
Kotera, Y.
et al. (2020)
[29]
moderate
Lee, I. et al.
(2016)
low
[31]
Lee, I. et al. low
(2017)
[32]
Study Population
Indications
Healthy adults, adults with
health conditions:
hypertension
Cardiovascular
System
Healthy adults, adults with
health conditions:
hypertension
Healthy adults, adults with
health conditions: metabolic
syndrome, chronic stroke,
psychiatric disorders
(depressions), chronic
diseases, chronic pains,
alcoholism
Healthy adults, adults with
health conditions: metabolic
syndrome, depressive
tendencies, chronic diseases
Cardiovascular
system
Mental health
Mental health
Children/adolescents with Atopic
atopic dermatitis
dermatitis
Healthy adults, adults with
health conditions:
alcoholism, COPD, chronic
stroke, hypertension, cancer,
mental disorders,
psychiatric inpatients or
outpatients, severe
depression
Mental health
Outcomes
Results
BLOOD PRESSURE:
systolic
(SBP)/diastolic
(DBP)
HEART RATE AND
PULSE RATE
DEPRESSION:
POMS; BDI; HDR;
DASS; EQVAS;
MMS
ANXIETY: POMS;
STAI; AAQ; DASS;
EQVAS
SBP (20 studies): ↓↓ in
forest group
DBP (17 studies): ↓↓ in
forest group
HR (5 studies)/PR (8
studies): ↓↓ in forest
group
DEPRESSION (20
studies): ↓↓ forest vs.
city
ANXIETY: (5 studies) ↓
after forest intervention,
(16 studies) ↓↓ after
forest intervention
ANGER: POMS
ANGER (14 studies): ↓↓
after forest intervention
ATOPIC
DERMATITIS:
SCORAD Index
(subjec-
tive/objective)
CHILD
ANXIETY-TEST
IMMUNOLOGY
BLOOD TEST:
TARC,
MDC,Serum
immune cytokine
levels
PHYSICAL
ACTIVITY: HPLP II
HEALTH
PROMOTION
BEHAVIOUR: HPLP
II
QUALITY OF LIFE:
EQ-VAS;
GHQ/QL-12,
SF-36,
WHOQOL-BREF,
POMS
ATOPIC DERMATITIS
SCORAD Index
(subjective/objective)
(all studies): all ↓↓
CHILD-ANXIETY-TEST
(1 study): ↓
IMMUNOLOGY BLOOD
TEST (1 study): WBC +
CD8+ T cells ↑↑;
Haemoglobin+ N cells
↓↓, all other ↔ ; TARC
(1 study): ↓; MDC (1
study): ↓↓; serum
immune cytokine levels
(1 study): IL-5 ↓↓; IL-2,
IL-4, IFN-y ↔
PHYSICAL ACTIVITY (1
study): ##
HEALTH PROMOTION
BEHAVIOUR (1 study): ##
QUALITY OF LIFE (5
studies): ##
POMS (15 studies): 14
studies ##, 1 study #
Int. J. Environ. Res. Public Health 2021, 18, 1770
13 of 38
Author
Table 2. Cont.
AMSTAR-2
Rating
Study Population
Indications
Healthy adults, adults with
health conditions:
alcoholism, COPD, chronic
stroke, hypertension, cancer,
mental disorders,
psychiatric inpatients or
outpatients, severe
depression
Mental health
Healthy adults, adults with
health conditions:
alcoholism, COPD, chronic
stroke, hypertension, cancer,
mental disorders,
psychiatric inpatients or
outpatients, severe
depression
Mental health
Healthy adults, adults with
health conditions:
alcoholism, COPD, chronic
stroke, hypertension, cancer,
mental disorders,
psychiatric inpatients or
outpatients, severe
depression
Mental health
Healthy adults, adults with
health conditions:
alcoholism, COPD, chronic
stroke, hypertension, cancer,
mental disorders,
psychiatric inpatients or
outpatients, severe
depression
Mental health
Outcomes
Results
DEPRESSION: BDI;
MADRS;
HDR-D17; Zung
Self-Rating
Depression Scale
ANXIETY: STAI
DEPRESSION (15
studies): 14 ##, 1 study #
ANXIETY (6 studies): 5
studies ##, 1 study #
STRESS: Stress
response,
inventory
measuring
self-reported stress
and arousal
HWA-BYUNG-
SYNDROME: The
Instrument of
Oriental Medical
Evaluation for
Hwa-Byung
STRESS:(2 studies): ##
HWA-BYUNG-
SYNDROME (1 study):
##
ANGER: STAXI
EMOTION: SD
-Method
ANGER (2 studies): ↔
EMOTION (4 studies): 3
studies ##, 1 study #
SELF-ESTEEM:
Self-esteem, The
Rosenberg
Self-Esteem Scale
SPIRITUALITY:
SHI, The Spiritual
Assessment Scale
RESILIENCE:
Self-regulation
Resilience
POS./NEG.
EFFECTS: PANAS,
ROS
SELF-ESTEEM (3 studies):
##
SPIRITUALITY (1 study):
##
RESILIENCE (1 study): ##
POS./NEG. EFFECTS (1
study): ##
Int. J. Environ. Res. Public Health 2021, 18, 1770
14 of 38
Author
Oh, B. et al.
(2017)
[19]
Table 2. Cont.
AMSTAR-2
Rating
low
Study Population
Indications
Outcomes
Results
Healthy adults, adults with
health conditions:
alcoholism, COPD, chronic
stroke, hypertension, cancer,
mental disorders,
psychiatric inpatients or
outpatients, severe
depression
Adults with health
conditions: hypertension
Healthy adults, adults with
health conditions: COPD
Healthy adults
Mental health
Cardiovascular
system
Immune and/or
inflammatory
indices
Immune and/or
inflammatory
indices
NK CELLS
BLOOD PRESSURE
SALIVARY
AMYLASE
(SALIVA/SERUM)
CORTISOL
PULSE RATE OR
HEART RATE
(PR/HR)
HRV/(IN LF/HF)
CYTOKINE: IL-6
ENZYME-BONDED
IMMUNOASSAY
BLOOD PRESSURE
HEART FUNCTION:
Cardio Ankle
Vascular Index
(CAVI)
IMMUNE
FUNCTION:
Expression von
Perforin (NK cells,
NK-similar cells,
CD8 + T cells) and
granzyme B
INFLAMMATION:
Proinflammatory
cytokines (IFN-y,
IL-6, IL-8, IL-1ß);
C-reactive protein
(CRP)
INFLAMMATION/
TUMOR: Tumor
necrosis factor α
ANTIOXIDANTS:
Biomarkers for
malondialdehyde
(MDA) and
superoxide
dismutase (SOD)
NK CELLS (1 study): ##
BLOOD PRESSURE (6
studies): 3 studies ##,
1 study #, 1 study n.a.
SALIVARY AMYLASE (2
studies): 1 study ##,
1 study #
(SALIVA/SERUM)
CORTISOL (4 studies): ##
PR OR HR (7 studies): 5
studies ##, 1 study #,
1 study n.a.
HRV (IN LF/HF) (8
studies): 5 studies ##,
2 studies #, 1 study n.a.
CYTOKINE (1 study)
IL-6: ##
ENZYME-BONDED
IMMUNOASSAY (1
study): ##
BLOOD PRESSURE (2
studies): ↓↓ in forest
group
HEART FUNCTION (1
study): ↑↑ in forest
group
IMMUNE FUNCTION (1
study): ↓↓ Perforin and
granzyme B in forest
groupINFLAMMATION:
Proinflammatory
cytokines (3 studies): ↓↓
in forest group; CRP (1
study): ↓ in forest group
INFLAMMATION/TUMOR
(2 studies): 1 study ↓↓ in
forest group, 1 study
↔
ANTIOXIDANTS (1
study): ↓↓ MDA in
forest group, SOD ↔
Int. J. Environ. Res. Public Health 2021, 18, 1770
15 of 38
Author
Song, M. K.
and Bang, K.
-S. (2017)
[34]
AMSTAR-2 Study Population
Rating
Older women
Table 2. Cont.
Indications
Lung function
Adults with chronic health
conditions: alcoholism,
fatigue syndrome
Mental health
Adults with health
conditions: fatigue
syndrome, COPD
Mental health
Healthy adults, adults
with health conditions:
hypertension, COPD
Mental health
Healthy children
Mental health
Healthy children
Healthy children
low
Mental health
Mental health
Healthy children
Mental health
Outcomes
Results
LUNG FUNCTION:
FEV1 (in 1 s) and
FEV6
(in 6 s)
ANXIETY AND
DEPRESSION:
BDI
HADS
STRESS: PSQserum
cortisol
LUNG FUNCTION: FEV
(in 1s) and FEV (in 6s) (1
study): ↑↑ in forest
group
ANXIETY AND
DEPRESSION: BDI (1
study):
↓↓ forest group
HADS (1 study): both
groups ↓↓,
↔ between groups
STRESS:
PSQ
(1 study): ↓ in forest
group
cortisol (1 study): ↓↓ in
forest group
MOOD: POMS
MOOD (3 studies): all ↑↑
in forest group
DEPRESSION: CDI;
Scale for Mental
Health Measurement
ANXIETY: STAI-C;
Scale for Mental
Health measurement
STRESS: Stress
Recognition
Inventory for
School-aged
Children; saliva
cortisol level; AMHI
SELF-ESTEEM:
Self-esteem
scale/self-esteem
NEGATIVE
EMOTIONS: Draw a
Story (DAS); scale
for emotional and
social development
test
ANGER: Novaco
Anger Scale
IMPULSIVENESS:
Scale for
mental-health
measurement
AGGRESSION: Scale
for aggression; scale
for mental health
measurement
ATTACK: Scale for
mental health
measurement
DEPRESSION (4 studies):
2 studies ##,
2 studies #
ANXIETY (3 studies): 2
studies ##, 1 studies #
STRESS (3 studies): 1
study stress recognition
##; 1 study salivary
cortisol ##; 1 study
AMHI stress level #
SELF-ESTEEM (3 studies):
##
NEGATIVE EMOTIONS (2
studies): ##
ANGER (1 study): ##
IMPULSIVENESS (2
studies): 1 study ##; 1
study #
AGGRESSION (2 studies):
##
ATTACK (1 study): #
Int. J. Environ. Res. Public Health 2021, 18, 1770
16 of 38
Author
AMSTAR-2 Study Population
Rating
Healthy children
Healthy children
Healthy children
Healthy children
Healthy children
Healthy children
Table 2. Cont.
Indications
Outcomes
Results
Mental health
Mental health
Mental health
Mental health
Sociality
Sociality
MENTAL HEALTH:
AMHI; scale for
mental-health
measurement;
scale for
psychological,
social, moral, and
physical level
SUBJECT
WELL-BEING:
Subject Well-being
Scale
PSYCHOLOGICAL
SKILLS: Emotional
Intelligence Test;
AMHI;
Ergo-Resilience
Scale
PHYSICAL SKILLS:
Scale for
psychological,
social, moral, and
physical level
SOCIALITY:
Korean Personality
Inventory: sociality
SOCIAL
COMPETENCE:
Social Competence
Scale; scale for
emotional and
social
development test;
scale for
psychological,
social, moral, and
physical level
SCHOOL
VIOLENCE
ATTITUDE: Scale
for school violence
attitude
SCHOOL
ADJUSTMENT:
Scale for school
adjustment;
multiple life
satisfaction
scaleLIFE RESPECT:
Scale for life
respect
MENTAL HEALTH (4
studies): 2 studies #;
1 study mental health
quotient ##;
1 study psychological
level ##
SUBJECT WELL-BEING (1
study): #
PSYCHOLOGICAL SKILLS
(3 studies): 1 study
Ergo-Resilience Scale:
interpersonal
relationship and
curiosity ##.; 1 study
emotional intelligence
##; 1 study possibility of
problem behaviour
(chronic fatigue) and
psychological resources
##
PHYSICAL SKILLS (1
study): ##
SOCIALITY (2 studies):
##
SOCIAL COMPETENCE (3
studies): ##
SCHOOL VIOLENCE
ATTITUDE (1 study): ##
SCHOOL ADJUSTMENT:
(2 studies):
both in parts ##
LIFE RESPECT (1 study):
##
Int. J. Environ. Res. Public Health 2021, 18, 1770
17 of 38
Table 2. Cont.
Author
Antonelli, M.
et al. (2019)
[27]
Wen, Y. et al.
(2019)
[36]
AMSTAR-2
Rating
low
low
Study Population
Healthy children, adults
with health conditions:
COPD, high risk for
stress/burnout, severe
depression, hypertension,
postmenopausal women
Healthy children/adults,
adults with health
conditions: hypertension,
COPD, chronic stroke,
chronic heart failure
Healthy adults, adults with
health conditions:
hypertension
Healthy adults, adults with
health conditions:
hypertension, COPD,
chronic heart failure
Adults with health
conditions: chronic heart
failure
Indications
Outcomes
Mental health
STRESS:
salivary/serum
cortisol
Cardiovascular
system
BLOOD PRESSURE:
SYS-
TOLIC/DIASTOLIC
HEART RATE
PULSE RATE
HRV
Metabolic
parameters
TRIGLYCERIDE
ADIPONECTIN
Immune and/or
inflammatory
indices
NK CELLS
NKT CELLS
INTERLEUKIN
(IL-6, IL-8)
TUMOR NECROSIS
FACTOR
CRP
Immune and/or
inflammatory
indices
ANTIOXIDANTS:
Glutathione
peroxidase
biological
antioxidant
potential;
peroxides
(8-hydroxy-2’-
deoxyguanosine
and hydrogen);
MDA
HYPERVENTILA-
TION
Results
STRESS (22 studies): 20
studies ↓↓ forest vs.
non-forest
within group: 13 studies
↓↓, 1 study ↑↑, 5 n.a.
between groups: 13
studies ↓↓ forest vs.
non-forest, 1 ↑↑ forest vs.
non-forest, 4 ↔ , 3 n. a.
BLOOD PRESSURE (8
studies): ↓↓ in 5 studies
in forest group, 1 study
↓↓ between groups,
1 study ↑↑ between
groups, 1 study irregular
index
HEART RATE (3 studies):
all ↓↓ between groups
PULSE RATE (5 studies):
↓↓ in 4 studies, 1 study ↓;
HRV (6 studies): lnHF
↑↑ in 4 studies,
1 study ↓; lnLF/lnHF ↓↓
in 2 studies,
1 study ↓, 2 studies ↑
TRIGLYCERIDE (2
studies): ↓↓
ADIPONECTIN (1 study):
↑↑
NK CELLS (2 studies):
↓↓
NKT CELLS (1 study):
↓↓;
INTERLEUKIN (4
studies): in 3 studies ↓↓
TUMOR NECROSIS
FACTOR (3 studies):
2 studies ↓↓
CRP (3 studies): 1 study
↓↓
ANTIOXIDANTS:
Glutathione peroxidase
(1 study): ↑↑, biological
antioxidant potential (1
study): ↑↑, Peroxides (1
study): ↓↓, MDA (2
studies): ↓↓
HYPERVENTILATION (2
studies): ↓↓
Int. J. Environ. Res. Public Health 2021, 18, 1770
18 of 38
Author
Chae, Y. R.
et al. (2018)
[35]
AMSTAR-2 Study Population
Rating
Table 2. Cont.
Indications
Healthy adults, adults with
health conditions:
hypertension, COPD
Mental health
Healthy adults
Mental health
Healthy adults, adults with
health conditions:
hypertension, COPD,
chronic heart failure
Mental health
Healthy adults, adults with
health conditions:
hypertension
Mental health
Healthy children/adults,
adults with health
conditions: chronic stroke
Mental health
Healthy adults
Mental health
Healthy children/adults
Mental health
critically
low
Healthy adults
Healthy adults
Metabolic
parameters
Menopausal
symptoms
Outcomes
Results
STRESS: Stress
management;
stress reaction;
cortisol;
adrenaline;
norepinephrine;
dopamine
STRESS (6 studies):
management 1 study ↑↑
between groups;
reaction 1 study ↓↓
between groups;
hormones (5 studies):
2 studies ↓↓ within
group,
3 studies ↓↓ between
groups
ELECTROPHYSIOLOGICAL
INDICES:EEG, high
alpha brain waves
and high beta
ELECTROPHYSIOLOGICAL
INDICES (1 study): ↑↑
brain waves
POMS (14 studies): in 11
studies ↓↓ negative
POMS
emotions, 10 studies ↑↑
tension, 2 studies ↑↑
positive emotions
ATTITUDES AND
FEELINGS ABOUT
THINGS: SD
method
ATTITUDES AND
FEELINGS ABOUT
THINGS (6 studies): in 5
studies ↑↑; 1 study n.a.
ANXIETY AND
DEPRESSION: BDI,
HDR, CDI, STAI
ANXIETY (6 studies): 4
studies ↓↓ within group,
3 studies ↓↓ between
groups
DEPRESSION (3 studies):
2 studies ↓↓ within
group, 2 studies ↓↓
between groups
DEGREE OF
PHYS./PSYCH.
REGENERATION:
Somatic Quality of
Life: EQ-5D-3L;
somatic symptoms;
psychological
regeneration;
mental health
DEGREE OF
PHYS./PSYCH.
REGENERATION:
Somatic Quality of life (1
study): ↑↑ within group
somatic symptoms (2
studies): ↓↓
psychological
regeneration, mental
health (2 studies): ↑↑
ADAPTIVE
BEHAVIOUR:Self-
esteem;
health-promoting
behaviour
ADAPTIVE BEHAVIOUR:
self-esteem (1 study): ↑↑
health-promoting
behaviour (1 study): ↑↑
TRIGLYCERID
LEVEL
TRIGLYCERID LEVEL (1
study): ↓↓
MENOPAUSAL
COMPLAINTS:
Menopausal
symptoms
MENOPAUSAL
COMPLAINTS:
Menopausal symptoms
(1 study): ↓
Int. J. Environ. Res. Public Health 2021, 18, 1770
19 of 38
Table 2. Cont.
Author
AMSTAR-2
Rating
Putra, R. et al.
(2018)
[33]
critically
low
Study Population
Healthy adults: adults with
health conditions: alcohol
dependency
Healthy adults: adults with
health conditions: alcohol
dependency; Hwa-Byung;
depression; cancer; mild
cognitive impairment
Healthy adults: adults with
health conditions:
Hwa-Byung; depression;
mild cognitive impairment
Healthy adults: adults with
health conditions: alcohol
dependency
Healthy adults: adults with
health conditions:
Hwa-Byung; depression;
mild cognitive impairment
Healthy adults
Indications
Outcomes
Results
Mental health
Mental health
STRESS:
Employment/job
stress;
psychosocial stress
STRESS (8 studies): all ↓
DEPRESSION: BDI;
HDR; MADRS
ANXIETY: n.a.
DEPRESSION (9 studies):
all ↓
ANXIETY (7 studies): 4
studies ↓, 2 studies ↔
Quality of Life
QUALITY OF LIFE:
SF-36; QoL
QUALITY OF LIFE (4
studies): all ↑
Mental health
EMOTION: POMS EMOTION (2 studies): ↑↑
Mental health
HEART RATE
VARIABILITY
(HRV)
Immune and/or
inflammatory
indices
IMMUNE
FUNCTION: NK
activity;
adrenaline
concentration in
urine;
salivary/serum
cortisol
BLOOD PRESSURE
PULSE RATE (PR)
HRV
WBC
POMS
HRV (2 studies): ↑
IMMUNE FUNCTION:
NK activity (4 studies):
all ↑↑ in forest group,
adrenaline (4 studies): 2
studies ↓↓ in forest
group, 1 study ↔ , 1
study ↑↑;
cortisol (5 studies): 3
studies ↓↓, 1 study ↔
in forest group, 1 study
↓ in both groups
BLOOD PRESSURE (4
studies): 1 study ↔ ,
2 studies ↓↓ in forest
group, 1 study n.a.
PULSE RATE (5 studies):
3 studies ↓↓, 1 study
unchanged, 1 study ↑↑
in forest group
HRV (3 studies): 1 study
↑↑, 1 study ↓↓,
1 study ↔ in forest
group
WBC (4 studies): 2
studies ↔ , 2 studies n.
a.
POMS (4 studies): all ↑↑
in forest group
Int. J. Environ. Res. Public Health 2021, 18, 1770
20 of 38
Table 2. Cont.
Author
AMSTAR-2 Study Population
Rating
Indications
Outcomes
Results
Farrow, M. R.
and
Washburn, K.
(2019)
[30]
critically
low
Healthy adults
Mental health
Healthy adults, adults with
health conditions:
hypertension
Mental health
ACTIVITY OF THE
PARASYMPA-
THETIC NERVOUS
SYSTEM: HRV
(InLF/HF, InHF)
BLOOD PRESSURE
PULSE RATE
SALIVARY
CORTISOL LEVEL
DOPAMINE/
ADRENALINE/
NORADRENALIN
IN URINE
ANXIETY (POMS
subscale values,
SD Method)
ACTIVITY OF THE
PARASYMPATHETIC
NERVOUS SYSTEM: ↑↑
InHF, ↓↓ lnLF/HF
BLOOD PRESSURE (2
studies): ↓
PULSE RATE (6 studies):
↑
SALIVARY CORTISOL (3
studies): ↓
Adrenaline in urine (1
study): ↓
ANXIETY (8 studies): ↓
↓↓ significantly reduced; ↓ reduced, not significant; ↑↑ significant improvement; ↑ improvement, not significant; ↔ unchanged; ##
significant change—not specified by authors; # change, not significant—not specified by authors; AAQ: Anti-Anxiety Questionnaire; AMHI:
Adolescent Mental Health Inventory; BDI: Beck Depression Inventory; CDI: Children’s Depression Inventory; COPD: chronic obstructive
pulmonary disease; CRP: C-reactive protein; DAS: Draw a Story; DASS: Depression Anxiety and Stress Scale; DBP: diastolic blood pressure;
EEG: electroencephalogram; EQVAS: EuroQol Visual Analog Scale; EQ-5D-3L: European Quality of Life 5 Dimensions 3 Level Version;
GHQ/QL-12: General Health Questionnaire/Quality of Life; HADS: Hospital Anxiety and Depression Scale; HDR: Hamilton Depression
Rating Scale; HPLP II: Health-Promoting Lifestyle Profile II; HR: heart rate; HRV: heart rate variability; Hwa-Byung: Korean culture-
induced anger syndrome with symptoms of insomnia, depression, and somatisation in the lower abdomen; MADRS: Montgomery–Åsberg
Depression Rating Scale; MDA: malondialdehyde biomarkers; MDC: macrophage-derived chemokine; MMS: Multiple Mood Scale; NK
cells: natural killer cells; PANAS: Positive and Negative Affect Schedule; POMS: Profile of Mood States; PR: pulse rate; ROS: The Restorative
Outcome Scale; SBP: systolic blood pressure; SCORAD: Scoring Atopic Dermatitis; SD Method: Semantic Differential Method; SF-36:
short form health 36; SHI: Spiritual Health Inventory; SMHM: Scale for Mental Health Measurement; SOD: superoxide dismutase; STAI:
The Spielberger State–Trait Anxiety Inventory; STAXI (-C): State–Trait Anger Expression Inventory (for children); TARC: thymus and
activation-regulated chemokine; WBC: white blood cell count; WHOQOL-BREF: WHO Quality of Life–BREF.
Table 3. Summary of associations between forest-based interventions and health effects/outcomes on the cardiovascu-
lar system.
Health
Effects/Outcomes
Forest-Based Interventions
Reference of
Association (+)
Blood pressure
Walking/sitting in and viewing
forest area
Walking in forest area
Ideno, Y. et al. (2017) [28]
Oh, B. et al. (2017) [19]
Walking/activity/rest in forest area Wen, Y. et al. (2019) [36]
Walking/activity/rest in forest area Wen, Y. et al. (2019) [36]
Heart and pulse rate
Sitting in and viewing forest
area/walking and activities in the
forest
Ideno, Y. et al. (2017) [28]
Cardio Ankle Vascular
Index (CAVI)
Walking in forest area
Oh, B. et al. (2017) [19]
HRV
Walking/activity/rest in forest area Wen, Y. et al. (2019) [36]
HRV: heart rate variability; +: mainly an improvement; +/−: mixed results.
Reference of
Association (+/−)
Int. J. Environ. Res. Public Health 2021, 18, 1770
21 of 38
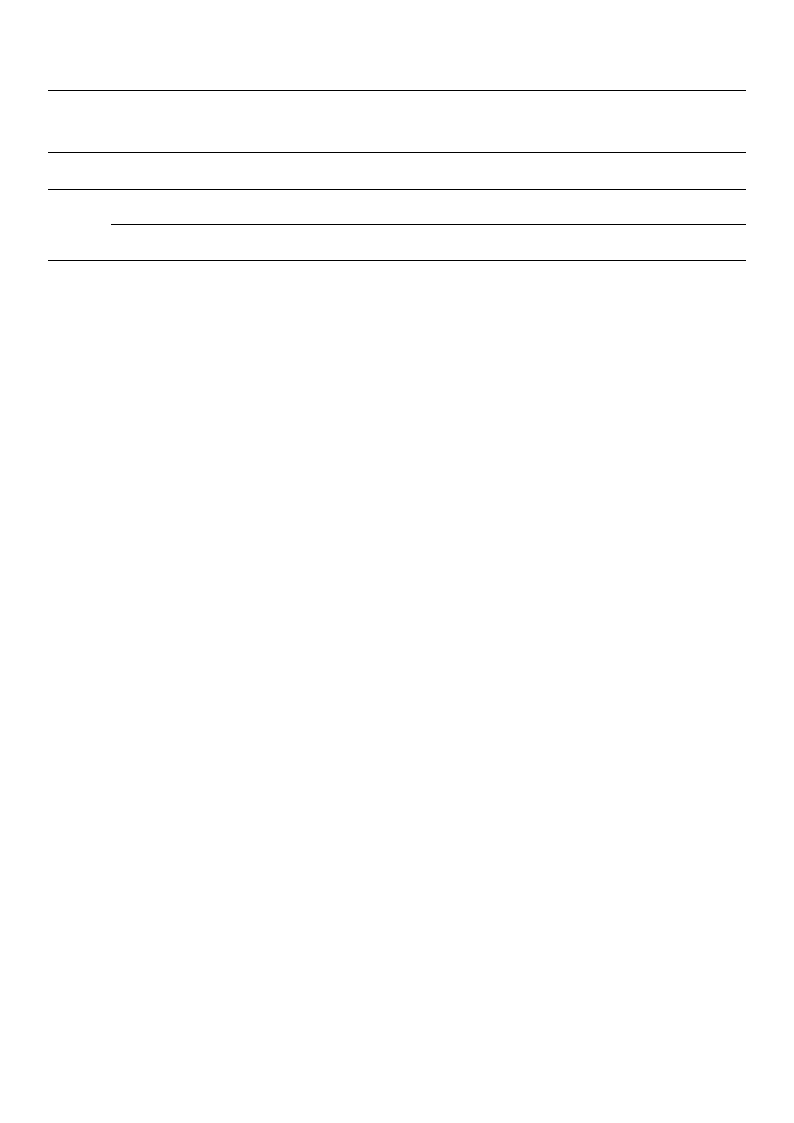
Table 4. Summary of associations between forest-based interventions and health effects/outcomes in immune and inflam-
matory parameters.
Health Effects/
Outcomes
Forest-Based Interventions
Reference of
Association (+)
Reference of
Association (+/−)
NK/NKT cells
Walking in forest area
Walking in forest area
Oh, B. et al. (2017) [19]
Wen, Y. et al. (2019) [36]
Cytokines
Walking in forest area
Walking in forest area; exposed to
forest
Oh, B. et al. (2017) [19]
Wen, Y. et al. (2019) [36]
CRP
Walking in forest area
Oh, B. et al. (2017) [19]
Walking in forest area
Wen, Y. et al. (2019) [36]
Tumour necrosis factor
Walking in forest area
Walking in forest area; exposed to
forest
Oh, B. et al. (2017) [19]
Wen, Y. et al. (2019) [36]
Antioxidants
Walking in forest area
Walking and meditation in forest area;
exposed to forest
Wen, Y. et al. (2019) [36]
Oh, B. et al. (2017) [19]
CRP: C-reactive protein; NK cells: natural killer cells/NKT cells: natural killer T-cells; +: mainly improvement; +/−: mixed results.
Table 5. Summary of associations between forest-based interventions and health effects/outcomes in
metabolic parameters.
Health Effects/
Outcomes
Forest-Based
Interventions
Triglyceride
level
Walking in forest area
Adiponectin
level
Walking in forest area
+: mainly improvement; +/–: mixed results.
Reference of
Association (+)
Wen, Y. et al. (2019)
[36]
Wen, Y. et al. (2019)
[36]
Reference of
Association
(+/–)
Table 6. Summary of associations between forest-based interventions and health effects/outcomes in
atopic dermatitis.
Health Effects/
Outcomes
Forest-Based Interventions
Reference of
Association
(+)
Reference of
Association
(+/–)
SCORAD
Index
Forest experience, forest trip;
forest activity; forest camp;
forest camp swimming
Forest trip; forest activity;
forest camp
Lee, I. et al.
(2016) [31]
Lee, I et al.
(2016) [31]
SCORAD Index: Scoring Atopic Dermatitis Index; +: mainly improvement; +/–: mixed results.
Int. J. Environ. Res. Public Health 2021, 18, 1770
22 of 38
Table 7. Summary of associations between forest-based interventions and health effects/outcomes in mental health.
Health Effects/
Outcomes
Stress(cortisol
level/PROs)
Anxiety and
depression (PROs)
Negative
emotions(PROs)
Quality of life/well-
being(PROs)
Forest-Based Interventions
Walking in forest area; forest healing
program
Forest healing program (with
cognitive behavioural rehabilitation)
Forest activity; forest healing program
Walking/activity/rest in forest area
Forest bathing: spending time in a
forest, walking, resting, watching, and
deep breathing for a limited time in
forest
Walking in forest area, resting in the
forest, forest healing program, forest
therapy
Forest healing program (with
cognitive behavioural rehabilitation)
Activity in forest area, forest
experience program
Walking/activity/mediation/rest in
forest area
Waking, mediation in forest area,
forest therapy program
Walking, activity, resting in forest area,
forest experience program
Walking in forest area
Activity in forest area, forest
experience program, forest ecology
exploration
Walking/activity/rest in forest area
Walking, resting/breathing in forest
area, recreation program, forest
therapy program, forest bathing
program
Walking in the forest; forest-healing
program, forest therapy
Reference of
Association (+)
Lee, I. et al. (2017) [32]
Oh, B. et al. (2017) [19]
Song, M. K. and Bang,
K. -S. (2017) [34]
Wen, Y et al. (2019) [36]
Antonelli, M. et al.
(2019) [27]
Lee, I. et al. (2017) [32]
Oh, B. et al. (2017) [19]
Wen, Y. et al. (2019) [36]
Kotera, Y. et al. (2020)
[29]
Lee, I. et al. (2017) [32]
Oh, B. et al. (2017) [19]
Song, M. K. and Bang,
K. -S. (2017) [34]
Wen, Y. et al. (2019) [36]
Kotera, Y. et al. (2020)
[29]
Lee, I. et al. (2017) [32]
Activities in the forest
Walking/activities in the forest
Wen, Y. et al. (2019) [36]
PRO: patient reported outcome; +: mainly improvement; +/−: mixed results.
Reference of
Association (+/−)
Song, M. K. and Bang,
K. -S. (2017) [34]
Song, M. K. and Bang,
K. -S. (2017) [34]
Table 8. Summary of associations between forest-based interventions and health effects / outcomes in sociality.
Health Effects / Outcomes
Sociality(PRO)
Social Competence (PROs)
School Violence Attitude
(PRO)
Forest-based
Interventions
Forest-experience program,
forest-therapy program
Forest-healing program,
ecology exploration
Forest-ecology exploration
Reference of
Association (+)
Song, M. K. & Bang, K.-S.
(2017) [32]
Song, M. K. & Bang, K.-S.
(2017) [32]
Song, M. K. & Bang, K.-S.
(2017) [32]
Reference of
Association (+/–)
Int. J. Environ. Res. Public Health 2021, 18, 1770
23 of 38
Table 8. Cont.
Health Effects / Outcomes
Forest-based
Interventions
Reference of
Association (+)
School Adjustment (PROs)
Activities in the forest;
forest-experience program
Life Respect (PRO)
Forest-therapy program
Song, M. K. & Bang, K.-S.
(2017) [32]
PRO: Patient Reported Outcome; +: mainly improvement; +/–: mixed results.
Reference of
Association (+/–)
Song, M. K. & Bang, K.-S.
(2017) [32]
Most of the SRs and MAs included examined effects of forest-based interventions on
specific indications or indication areas [27,29–34]. Three papers were broader in scope.
They investigated the health effects of forest-based interventions without focusing on
one specific indication or indication area [19,35,36]. The individual studies included in
the reviews examined the effects of forest-based interventions mainly on the basis of
surrogate endpoints (blood pressure, saliva/serum cortisol, immune and/or inflammation
parameters, and other laboratory values). Patient-relevant endpoints are only found in the
studies on skin diseases (atopic dermatitis) and mental health.
The evaluation of the evidence on the impact of forest-based interventions on different
health outcomes summarised below is based not only on the study results, but also on
criteria, such as the study designs used, the sample sizes, the distribution of age and/or
gender in the study populations, the implementation of follow-up assessments, the study
quality/risk of bias, and the number of included studies on the respective topic.
3.4.1. Cardiovascular System
Three systematic reviews [19,28,36], one including a meta-analysis [28], reported on
the effectiveness of forest-based interventions on the cardiovascular system in healthy
people, as well as in adults with various previous diseases, such as hypertension. The
higher-quality review by Ideno et al. [28] contains 20 studies on cardiovascular issues.
Oh et al. [19] contains two studies, both of which are also included in Ideno et al. The
review by Wen et al. contains eight studies on the topic, one of which is already in-
cluded in Ideno et al. On the basis of the higher-quality review [26], we found that
forest-based interventions showed positive effects on blood pressure and heart and pulse
rates (Tables 2 and 3). This was also seen in the lower-quality reviews. The results were
confirmed by the meta-analysis by Ideno et al. The calculations using random-effects mod-
els showed statistically significant improvements with only slight heterogeneity among
studies (SBP: mean difference (MD) = −3.15, 95% confidence interval (CI) [−4.12; −2.18],
Heterogeneity (I2) = 1%; DBP: MD = −3.84, 95% CI [−5.27; −2.40], I2 = 24%; heart and
pulse rate: MD = −1.75, 95% CI [−2.38; −1.13], I2 = 39%). Most of the individual studies
on this topic were either non-randomised controlled trials with a cross-over design or ran-
domised controlled trials. Limitations are often very small sample sizes (<30), unbalanced
age, and/or gender distributions and the lack of follow-up (Table 1). There is also a high
risk of selection bias and high risks for performance and detection bias due to the lack of
blinding. As a result, there was evidence of short-term effects of forest-based interventions
on cardiovascular parameters, which was confirmed by Ideno et al., whose review had the
highest quality [28].
3.4.2. Immune and/or Inflammatory Parameters
Three reviews of low and critically low quality [19,33,36] reported the effects of forest-
based interventions on the immune system in healthy people, as well as in adults with
various previous diseases, such as COPD or chronic heart failure. In most individual
studies, an increase in natural killer (NK) or NKT cells and a decrease in cytokines and
CRP were observed after the intervention. However, the results on changes in antioxidants
and tumour necrosis factor α were inconsistent (Tables 2 and 4). The critically low-quality
review by Putra et al. [33] contains 10 individual studies on immune function, but these

Int. J. Environ. Res. Public Health 2021, 18, 1770
24 of 38
were described very inadequately and were not assessed for quality. This review could,
therefore, not be used to meaningfully evaluate the evidence on the impact of forest-
based interventions on the immune system. The work by Oh et al. [19] contains three
individual studies, and that by Wen et al. [36] contains six studies on the topic. One of
these studies is included in both reviews. All but one of the eight individual studies that
investigated immunological parameters were randomised controlled trials. Methodological
limitations included small sample sizes; skewed distributions in the age and/or gender
of study participants; and, to a large extent, the lack of follow-up. (Table 1). Overall, on
the basis of two low-quality reviews by Oh et al. and Wen et al., we found that there is
evidence suggesting at least a short-term effect of forest therapy on some immunological
and inflammation-related parameters.
3.4.3. Metabolic Parameters
One review of low and one of critically low quality [35,36] examined the effects of
forest-based interventions on metabolic parameters in healthy and hypertensive people.
Due to its considerable methodological weaknesses (such as no quality assessment/risk
of bias assessment for the included individual studies), the validity of the review of
critically low quality by Chae et al. [35] on the effects of forest therapy in terms of changing
metabolic parameters must be regarded as low. Wen et al. [36] reported on two studies
that investigated the change in metabolic parameters after forest-based interventions and
showed significant improvements in triglyceride and adiponectin levels (Tables 2 and 5).
Both were non-randomised controlled studies. The samples were small, the age and sex
distributions were distorted, and there was no follow-up (Table 1). Against this background,
the evidence for the effects of forest-based interventions on metabolic parameters is weak.
3.4.4. Atopic Dermatitis
One lower-quality review [31] reported the effectiveness of forest-based interventions
on the severity of atopic dermatitis in children and adolescents on the basis of the results
of five individual studies. The severity of atopic dermatitis assessed by the SCORAD index
improved significantly after intervention in four studies. No significance test was carried
out in the fifth study (Tables 2 and 6). Immunological blood tests showed divergent results.
All trials were uncontrolled (pre–post design), had small samples, and had no follow-up
(Table 1). The studies were also judged to be at high risk of detection bias due to the lack of
blinding of the assessors. In summary, there is only weak evidence for the effect of forest
therapy on the severity of atopic dermatitis in children and adolescents.
3.4.5. Mental Health
Stress
Five lower-quality reviews [19,27,32,34,36], one including a meta-analysis [27], re-
ported the effects of forest-based interventions on stress parameters in healthy people
and in adults with various previous diseases. The summaries of the results showed that
stress perception and stress hormones had significantly improved in the forest groups
after intervention in nearly all individual studies (Tables 2 and 7). Antonelli et al. [27]
additionally performed a meta-analysis (fixed-effects model) on the basis of the results
from eight selected RCTs. The reported effects on changes in saliva or serum cortisol
levels as stress biomarkers were very small overall, while there was great heterogeneity
among studies. Statistically significant effects were only observed in the subgroup Forest
Watching. No effect was found for the overall group and the subgroup Forest Walking
(overall: MD = −0.02, 95% CI [−0.05; 0.01], I2 = 81%; Forest Walking: MD = 0.03, 95% CI
[−0.01; 0.08], I2 = 50%; Forest Watching: MD = −0.05, 95% CI [−0.08; −0.01], I2 = 84%). The
asymmetry in the funnel plots also indicated a potential risk of publication bias. Antonelli
et al. judged the risk of performance bias to be high, but for other types of bias to be unclear
or low.

Int. J. Environ. Res. Public Health 2021, 18, 1770
25 of 38
Anxiety and Depression
Four low-quality [19,32,34,36] and one moderate-quality reviews, the latter including
meta-analyses [29], examined the effects of forest-based interventions on depressive symp-
toms and anxiety in healthy children and adults and in adults with various pre-existing
conditions. Significant improvements in depressive symptoms were found in almost all the
primary studies (Tables 2 and 7). Similar results were found for anxiety. The meta-analyses
(random effects model) by Kotera et al. [29] on depressive symptoms yielded small, but
statistically significant, mean effect estimates with a high degree of heterogeneity among
studies (RCTs: MD = −2.54, 95% CI [−3.56; −1.52], I2 = 87%; pre–post: MD = −1.04,
95% CI [−1.47; −0.60], I2 = 95%). All RCTs on depression had positive effects, i.e., depres-
sive symptoms decreased more in the forest than in the city after the interventions. The
meta-analysis of five RCTs on anxiety resulted in a large, but not significant, mean-effect
estimator (MD = −8.81, 95% CI [−21.91; 3.57], I2 = 97%). In the meta-analysis of 16 uncon-
trolled studies on anxiety, the mean effect estimator achieved was small, but statistically
significant, and there was also great heterogeneity among the studies (MD = −1.83, 95% CI
[−3.07; −0.58], I2 = 98%).
Negative Emotions
The same five reviews [19,29,32,34,36] examined the effects of forest-based interven-
tions on negative emotions, such as anger or aggression, in healthy children and adults and
in adults with various pre-existing conditions. Participants showed a significant decrease
in negative emotions after the forest-based interventions in most studies (Tables 2 and 7).
No changes could be found in some studies. The meta-analyses (random effects model)
by Kotera et al. [29] on four RCTs and 12 pre-post studies on anger achieved small but
statistically significant mean effect estimates with great heterogeneity among the studies
(RCTs: MD = −1.63, 95% CI [−13.25; −0.01], I2 = 88%; pre–post: MD = −0.81, 95% CI
[−1.17; −0.45], I2 = 93%). In summary, forest therapy seems to have positive effects on
emotional states, such as anger, aggression, impulsiveness, and rage in children, and in
healthy and pre-diseased adults.
Quality of Life/Well-Being
Three lower-quality reviews [32,34,36] reported on the impact of forest-based inter-
ventions on the health-related quality of life in healthy children and adults and in adults
with severe depression and in psychiatric patients. Significant changes in health-related
quality of life after forest-based interventions in adults could be shown (Tables 2 and 7).
One primary study included in the review by Song and Bang could not detect any change
in the well-being of healthy children after an eight-week forest-based intervention [34].
Mental Health—Conclusion
Six reviews [19,27,29,32,34,36], two including meta-analyses [27,29], reported the
impact of forest-based interventions on various aspects of mental health, including stress,
anxiety, depression, negative emotions, and quality of life/well-being (Tables 2 and 7).
Confidence in the results of the reviews according to AMSTAR-2 was rated as moderate
in one review [29] and as low in the other five reviews (Figure 3). On the basis of the
better-quality SRs and MAs, we found that the meta-analyses on depression revealed
small but statistically significant mean effect estimates with great heterogeneity among
studies [29]. In the lower-quality SRs and MAs, the changes in saliva or serum cortisol
levels as stress biomarkers reported in the meta-analysis were very small overall, and there
was also great heterogeneity among the studies [27]. Many of the primary studies had
a non-randomised or uncontrolled design, the sample sizes were sometimes small, the
age and gender distribution were not always balanced, and there was no study with a
follow-up. The risk of bias that could have influenced the results of the primary studies was
assessed differently by the authors of the six reviews. The risk for selection, performance,
and detection bias was often considered high, while attrition and reporting bias seemed

Int. J. Environ. Res. Public Health 2021, 18, 1770
26 of 38
to be of little relevance. In summary, there is some evidence for the effectiveness of forest
therapy on mental health. Indications of beneficial effects are mainly found in the areas of
stress, depression, anxiety, and negative emotions.
3.4.6. Sociality
One lower-quality review [32] reported the impact of forest-based interventions on
social skills and sociality in healthy primary-school children based on the results of 15 in-
dividual studies (two additional studies did not include forest-based interventions). Sig-
nificant improvements were found in all outcomes after the respective intervention and
compared to the control groups (Tables 2 and 8). Significant changes could be observed
only in some parts of the scales used, i.e., in the ability to adapt to school. The interven-
tions in the primary studies included in this review were mostly forest-based programs
that went beyond the usual forest-therapy walks, meditation and stays in the forest and
included additional elements, such as psychotherapy, exercise therapy or water therapy
(Table 1). The psychotherapeutic elements were likely to play a substantial role in the
changes achieved. None of the primary studies had a randomised design, and there was a
high risk of biased results in most of the trials, e.g., because evaluators were not blinded
and major confounding variables had not been taken into account. Despite many positive
study results, the evidence on the impact of forest-based interventions on social skills
and sociality in healthy primary-school children is limited due to shortcomings in study
implementation and because of the specific interventions.
4. Discussion
Our review summarises the evidence from systematic reviews and meta-analyses
available for the health effects of forest-based interventions, including a comprehensive
evaluation of the methodological quality of the included studies. We identified and
synthesised a total of 11 publications with 131 included primary studies, mostly from
Asian countries.
There is some overlap among the identified reviews, both at the primary study level
(i.e., if the same primary study was included in more than one review) and at the review
level (more than one identified review on the same topic). In a review on reviews, this
can lead to a misinterpretation of results and overestimation of evidence [38]. Of the
131 primary studies, 32 (24.4%) were included in more than one review, of which 21 (16.0%)
were included in exactly two reviews. However, the included reviews/meta-analyses often
addressed different research questions and thus used different outcomes of the primary
studies considered. For example, Antonelli et al. [27] summarised the effects of forest-based
interventions on cortisol levels, whereas Ideno et al. [28] were interested in the effects of
the forest environment on blood pressure. The primary studies included in both reviews
overlapped. However, since the two reviews considered different outcomes from the
primary studies, their overlap did not affect the interpretation of results in our review. In
summary, we consider the risk of overestimating the evidence due to overlap to be low.
4.1. Key Findings from the Review—Summary of Evidence
The systematic reviews that summarised the effects of forest-based interventions on the
cardiovascular system consistently reported positive effects both for prevention in healthy
people and for the treatment of adults with various pre-existing conditions [19,28,36].
Forest-based interventions also showed positive short-term effects on immunological
and inflammation-related parameters [19,36]. The possible improvement of metabolic
parameters after forest-based interventions remains unclear, as this outcome has been
investigated in too few primary studies [35,36]. One review synthesised the impact of
forest-based interventions on the severity of atopic dermatitis in children and adolescents.
Although there were significant improvements in the clinical picture, the evidence of
the effect was weak due to partially divergent results and serious methodological short-
comings, including the study designs [31]. Regarding mental health, several reviews

Int. J. Environ. Res. Public Health 2021, 18, 1770
27 of 38
showed positive effects on stress, depression, and anxiety, as well as on negative emotions
in healthy people and adults with various pre-existing conditions after forest-based in-
terventions [19,27,29,32,34,36]. Some reviews also reported significant improvements in
health-related quality of life among adults [32,34,36]. A further review points, albeit with
limited evidence, to the benefits of forest therapy programs on social skills and sociality in
healthy primary school children [34].
4.2. Latest Work on the Topic
Several primary studies and four reviews [39–42] on the topic—conducted in China,
Italy, the USA, and Malaysia—were newly published during the few months in which
we carried out our systematic review of SRs and MAs. According to PROSPERO, a meta-
analysis of randomised controlled trials on the effects of forest-based interventions on
mental health is also currently being conducted in Korea [43], and a research group in
the UK registered an umbrella review on the health benefits of forest therapy in 2019 [44].
However, the topics of these newly published reviews remained more or less the same as
those covered in the previous reviews—the effects of forest bathing in hypertensive patients
(main findings: forest bathing interventions reduced blood pressure, lowered the pulse
rate, increased the power of heart rate variability (HRV), improved cardiac-pulmonary
parameters, improved metabolic function, induced a positive mood, reduced anxiety
levels, and improved quality of life) [39], the health benefits of forests in terms of stress
reduction and relaxation (main finding: positive association between forest exposure and
mental well-being, suggesting forests as being effective in lowering stress levels) [40], and
physiological and psychosocial effects of forest therapy (main finding: forest therapy plays
an important role in preventive medicine and stress management for all age groups) [42].
Only Hansen and Jones addressed a topic which, to our knowledge, has not been dealt with
in previous reviews, or at least not in a focused manner. In their review, they investigated
the relationship between Shinrin-Yoku and spirituality (main finding: nature may have a
positive effect on human spirituality and, therefore, can enrich individuals’ well-being) [41].
4.3. Mechanisms of Action
Forest bathing originated in Japan in the 1980s, and the practice is already much more
widespread there and in other Asian countries than in Europe. The question often arises as
to whether the health mechanisms in European forests are equivalent or at least comparable
to those in Asian forests [9,29,45,46]. Forests with a closed canopy are comparable because
they provide a special interior forest climate with reduced air temperature, high air purity
and humidity, and special light conditions. These climatic factors are beneficial to health
and relieve the respiratory tract and the thermoregulation system [11]. Another important
factor is the peace and quiet in forests, which is essential for mental recovery in a time
of acoustic stimulus overload in urban settings. It is assumed that the effect of biogenic
volatile organic compounds (BVOC) emitted by trees and plants, such as phytoncides
(also known as terpenes in German), has an influence on human health in terms of their
anti-inflammatory, antioxidant, or neuroprotective activities [47–49]. This has not yet
been conclusively clarified scientifically, but the authors of a recent state-of-the-art review
confirmed that inhaling forest VOCs can result in useful antioxidant and anti-inflammatory
effects on the airways. Other possible benefits mentioned include promoting brain function
by reducing mental fatigue, inducing relaxation, and improving cognitive performance
and mood. The authors emphasised that tree composition can significantly influence the
concentration of certain VOCs in forest air [50]. The scientific literature on forest-based
interventions too rarely describes the structure of the forests in which the interventions were
carried out. The different types of forests are rarely compared regarding their health effects,
making it almost impossible to compare forests both within a country and across continents.

Int. J. Environ. Res. Public Health 2021, 18, 1770
28 of 38
4.4. Strengths and Limitations
4.4.1. Strengths
The present systematic review on SRs and MAs across the globe provides the most
comprehensive summary of the currently available evidence on forest-based preventative
and therapeutic interventions. The systematic search in the major medical literature
databases was carried out without language restrictions. This was necessary, as many
primary studies and systematic reviews on the impact of forest-based interventions were
carried out in Asia and are often published in the local language. A further strength of
our review was the stringent quality assessment using a specific tool for the evaluation of
systematic reviews with and without meta-analyses.
4.4.2. Limitations at the Primary Study Level
The authors of the included reviews considered many of the included primary studies
to be of medium or poor quality or at (relatively) high risk of bias (Table 1). The most
common concern was the lack of blinding of participants, therapists, and/or assessors,
which can contribute to both performance and detection bias. Many of the included
primary studies were also characterised by a lack of reporting quality (e.g., insufficiently
described target groups and randomisation; confounding variables were not reported;
results were insufficiently reported; dropouts, randomisation, and/or blinding were not
reported), deficiencies in study design (e.g., small study populations; skewed distribution
of characteristics such as age or gender in the groups; unrepresentative results; no or
inadequate control groups; no follow-up; important confounding parameters were not
recorded; study dropouts were not considered; use of non-validated instruments), and
deficiencies in the conduct of the study.
4.4.3. Limitations at the Review Level
Most of the reviews included in the AMSTAR-2 evaluation were assessed as having low
or critically low confidence in the findings (Figure 3). Only studies from a single country—
usually South Korea—were included in several reviews [31,33–35]. The literature search
was mostly limited to publications written in English or additionally in the respective
national language. Many of the reviews lacked an a priori prepared study protocol; a
quality assessment of the included primary studies; and an independently conducted study
selection, data extraction, and quality assessment by at least two reviewers.
4.4.4. Limitations at the Overview Level
An overview of systematic reviews itself has methodologic limitations, such as the
potential loss of information due to repeated syntheses. Overviews of reviews depend
on the quality of the included systematic reviews and these depend on the quality of the
included primary studies. Ideally, only high-quality studies should be included in an
overview of reviews, but this is not realistically feasible for many issues.
We were unable to conduct literature searches in Korean, Japanese, or Chinese
databases. Thus, we may have missed a systematic review. However, since we used
seven major international medical databases and searched for systematic reviews (not for
single studies), we believe that we identified most for this comprehensive overview. We
also conducted a recent update and identified currently ongoing reviews (see Section 4.2).
Very recent findings may have been missed because recently published single studies could
not have been captured by the reviews included.
We automatically translated the three reviews written in Korean using Google Trans-
late. Since both the abstracts and the tables in these publications were available in English,
we consider this procedure to be legitimate and sufficiently valid. Nevertheless, it cannot
be ruled out that some information was not recognised or was misinterpreted.

Int. J. Environ. Res. Public Health 2021, 18, 1770
29 of 38
4.5. Implications for Practice and Future Research
4.5.1. Interventions
The forest-based interventions reported in the included SRs and MAs covered a
broad and heterogeneous range of activities. These range from individual forest-based
interventions, such as “experiencing the forest with all five senses”, to forest therapy
with several activities in the forest, such as walking, sitting, and observing, to complex
multimodal forest healing programs. The latter were also combined with sports activities
and/or therapeutic elements, such as psychotherapy, exercise therapy, water therapy, or
nutritional therapy in some studies.
There are no internationally agreed definitions of forest bathing, forest therapy, and
other forest-based interventions and programs. Both the goals and the contents of forest
therapy differ in the different countries. While in Japan, forest bathing is supposed to
help stressed-out people find peace of mind, the focus in South Korea is on general health
promotion and the enhancement of the common welfare through various forest programs
for all population groups [51]. In America, a connection to nature is to be established
through immersion in the forest environment [52].
In Japan, where Shinrin-Yoku has a decades-long tradition, it is defined as forest
bathing in specially selected forests with the aim of maintaining physical vitality and
mental health, as well as preventing disease. The focus is especially on stress reduction
and strengthening the immune system. The Forest Therapy Society of Japan attempts to
establish an international standard for practice through information events and training.
The definition and potential elements of forest therapy remain imprecise and very broad.
The forest should be experienced with all five senses during the forest bath/forest therapy.
Activities such as hiking/walking, but also mindfulness exercises for the perception of
the environment, can be practiced. Measures such as nutritional therapy can complement
these activities [53].
In summary, the interventions carried out under the labels “forest bathing” or “forest
therapy” are diverse and often difficult to compare. Stays in the forest, combined with
mindfulness exercises and perception exercises with all senses, constitute the core elements
of forest bathing/forest therapy. Additional activities, such as Nordic walking, hiking, and
swimming; psychotherapeutic measures; and nutritional therapy, which together often
resemble a multimodal approach from the naturopathic complex treatment, are obviously
not excluded. Future studies need to define and precisely describe these interventions,
especially when implementing such multimodal forest-based programs.
4.5.2. Selection of Control Groups for the Investigation of the Effects of
Forest-Based Interventions
Most primary studies with a control group examined the effects of forest-based inter-
ventions in comparison to the same interventions in an urban environment. These included
walks and meditation.
Some reviews also include primary studies with multimodal forest-based interven-
tions that go beyond the usual walks, meditation, and stays in the forest, and do not
differ significantly from a traditional, holistic approach from naturopathy with exercise,
nutrition, relaxation, and stress management. The effects achieved by such interventions,
often referred to as “forest healing programs”, were usually compared to control groups
without any specific intervention. Controls merely followed their “daily routine” [32,34].
These studies examined the health effects of complex forest-based interventions without
specifically addressing the contribution of the forest environment to the effects achieved.
It remains unclear as to whether the same complex interventions in an environment out-
side the forest would have led to the same results. The control group design used here
can, therefore, be described as inadequate for the investigation of the forest effect. It is
similar with a study included in the review by Wen et al. [36] in which participants with
neck pain received forest therapy. The intervention consisted of forest bathing in both the
control group and the intervention group. The intervention group additionally performed

Int. J. Environ. Res. Public Health 2021, 18, 1770
30 of 38
stretching and strengthening exercises [54]. This, too, is an example of an inadequate
control group, since this study design was used to investigate the effects of stretching and
strengthening exercises rather than forest therapy.
These examples show that special attention should be paid to a suitable control group
when choosing a study design to demonstrate the effects of forest bathing/forest therapy.
4.5.3. Recommendations for Practice and Future Research
The therapeutic effects of forest-based interventions on hypertension, stress, and
mental health disorders, such as depression and anxiety, have been demonstrated. Forest
therapy could also have a positive effect on the severity of atopic dermatitis in children.
However, these effects reported in a Korean review [31] need to be confirmed in better-
designed, controlled intervention studies. The effects on immunological and inflammation-
related parameters should be verified by studies in appropriate native forests.
Forest characteristics, such as terpene concentration, microbial diversity, biodiversity,
noise or quiet (psychoacoustics), light conditions, forest composition, and climatic factors,
should be included in studies. Many questions remain unanswered in this context. For
example, what kind of forest is needed for what objective? Do deciduous forests have a
different effect than coniferous forests (an initial pilot study by Karim et al. [13] suggests
differences)? How long does the stay in the forest have to last to have medium-to-long-term
effects in addition to the acute effects? Which groups of people or patients benefit most
from which intervention? Vulnerable groups, such as the elderly and/or people with
disabilities, should also be considered.
Target groups for preventative forest-based interventions are people under stress
and individuals with mental and emotional problems, particularly (a) elderly people (to
encourage participation and prevent falls), (b) individuals living alone, and (c) patients
in the rehabilitation phase at health resorts. To achieve sustainable effects, forest bathing
should be practiced several times a week.
5. Conclusions
The present systematic international review of SRs and MAs provides the most com-
prehensive summary of the currently available evidence on forest-based preventive and
therapeutic interventions.
Most of the systematic reviews did not reach an acceptable quality level after a
stringent assessment of their methods. The study designs, control groups, and study
populations of the included individual studies were often inadequate for the research
question under investigation, which considerably limits the contribution of the relevant
studies to the evidence in the research field.
The results of the better reviews showed that forest bathing may be beneficial for (1)
the cardiovascular system by lowering blood pressure and reducing the heart rate/pulse
rate in healthy adults and in people with hypertension and (2) mental health by reducing
stress and symptoms of depression and anxiety and decreasing anger in healthy adults and
in people with various health conditions. Forest therapy may also be beneficial for atopic
dermatitis in children. These effects need to be confirmed in well-designed, controlled
intervention studies. No considerable effects of forest-based interventions were seen for
changes in antioxidants and tumour necrosis factor α, sociality, and metabolic parameters.
In summary, the results suggest that forest-based interventions have a positive impact
on the cardiovascular system; some immunological and/or inflammatory parameters; and
mental health in the areas of stress, depression, anxiety, and negative emotions. Positive
effects were seen in healthy children and adults, as well as in adults with various pre-
existing conditions. The evidence for the effectiveness of forest-based interventions on
metabolic parameters in adults, on the severity of atopic dermatitis in children/adolescents,
and on social skills and sociality in healthy primary school children was weak. Since there
is no uniform use of the terms forest bathing (Shinrin-Yoku), forest therapy, and forest
medicine, future studies need to define and precisely describe their interventions.
Int. J. Environ. Res. Public Health 2021, 18, 1770
31 of 38
In the future, intervention studies with well-founded designs regarding the type
of study, control group, type and duration of the intervention, study population, and
description of the forest environment are required to improve our knowledge of forest-
based interventions for health promotion and therapeutic purposes. The sustainability of
the effects needs to be examined by sufficient post-intervention, follow-up assessments.
When conducting systematic reviews on the topic, additional attention should be paid to
methodologically careful study planning, implementation, and reporting.
Author Contributions: Conceptualisation, M.S.-J., V.T., A.S., D.F.; methodology, M.S.-J., V.T., M.K.;
formal analysis, V.T., M.K.; investigation, M.S.-J., V.T., M.K.; resources, G.I., A.S.; writing (original
draft preparation), M.S.-J., V.T., M.K.; writing (review and editing), all authors; project administration,
M.S.-J.; funding acquisition, D.F. All authors have read and agreed to the published version of
the manuscript.
Funding: This research was funded by the Bavarian State Ministry of Health and Care (Project#
LGL-GE8_2/2019), Germany.
Conflicts of Interest: The Chair of Public Health and Health Services Research (IBE) at the LMU
received study support (third-party funding for the research project). A.S. and G.I. are the authors of a
recently published book on forest therapy [11]. They also developed a scientifically based curriculum
for training in forest therapy and forest bathing in 2018. Since 2019, A.S. and G.I. have been teaching
health interventions in the preventive setting in the forest. A forest therapy seminar will follow in
2021. The authors declare no conflict of interest.
Appendix A. Search Strings
Table A1. Medline.
No.
1
2
3
4
5
6
7
8
9
10
11
12
Search Strings
“forest therap*”.ab,ti.
“forest bath*”.ab,ti.
forest medicine.ab,ti.
Shinrin-yoku.ab,ti.
forest healing.ab,ti.
“review*”.ab,ti.
“systematic*”.ab,ti.
“overview*”.ab,ti.
“Meta-Analys*”.ab,ti.
1 or 2 or 3 or 4 or 5
6 or 7 or 8 or 9
10 and 11
Hits
30
27
4
18
1
1,732,382
360,076
133,772
133,384
63
2,052,748
12
Table A2. Embase.
No.
Search Strings
Hits
1
“forest therap*”.ab,ti.
39
2
“forest bath*”.ab,ti.
45
3
forest medicine.ab,ti.
4
4
Shinrin-yoku.ab,ti.
21
5
forest healing.ab,ti.
4
Int. J. Environ. Res. Public Health 2021, 18, 1770
32 of 38
Table A2. Cont.
No.
6
7
8
9
10
11
12
Search Strings
“review*”.ab,ti.
“systematic*”.ab,ti.
“overview*”.ab,ti.
“Meta-Analys*”.ab,ti.
1 or 2 or 3 or 4 or 5
6 or 7 or 8 or 9
10 and 11
Hits
2,679,607
565,832
198,810
217,515
90
3,173,197
22
Table A3. Web of Science.
No.
# 12
# 11
# 10
#9
#8
#7
#6
#5
#4
#3
#2
#1
Search Strings
#11AND#10
#9OR#8OR#7OR#6
#5OR#4OR#3OR#2OR#1
TOPIC: (Meta-Analys*)
TOPIC: (overview*)
TOPIC: (systematic*)
TOPIC: (review*)
TOPIC: (forest healing)
TOPIC: (“Shinrin-yoku”)
TOPIC: (“forest medicine”)
TOPIC: (“forest bath*”)
TOPIC: (“forest therap*”)
Hits
64
3,453,809
470
196,262
331,638
889,313
2,509,712
287
112
3
70
68
Table A4. Cochrane Library.
No.
Search Strings
#1
(review*):ti,ab,kw OR (systematic*):ti,ab,kw OR (overview*):ti,ab,kw
OR (Meta-Analys*):ti,ab,kw (Word variations have been searched)
(forest NEXT therap*):ti,ab,kw OR (forest NEXT bath*):ti,ab,kw OR
#2
(Forest NEXT medicine):ti,ab,kw OR (Shinrin-Yoku):ti,ab,kw OR (forest
NEXT healing):ti,ab,kw (Word variations have been searched)
#3
#1 AND #2
Hits
91,743
27
0
Table A5. Psycinfo.
No.
Search Strings
S3
(S1 AND S2)
S2
review* OR systematic* OR overview* OR Meta-Analys*
S1
“forest therap*” OR “forest bath*” OR “forest medicine” OR
“shinrin-yoku” OR “forest healing”
Hits
2
776,703
12
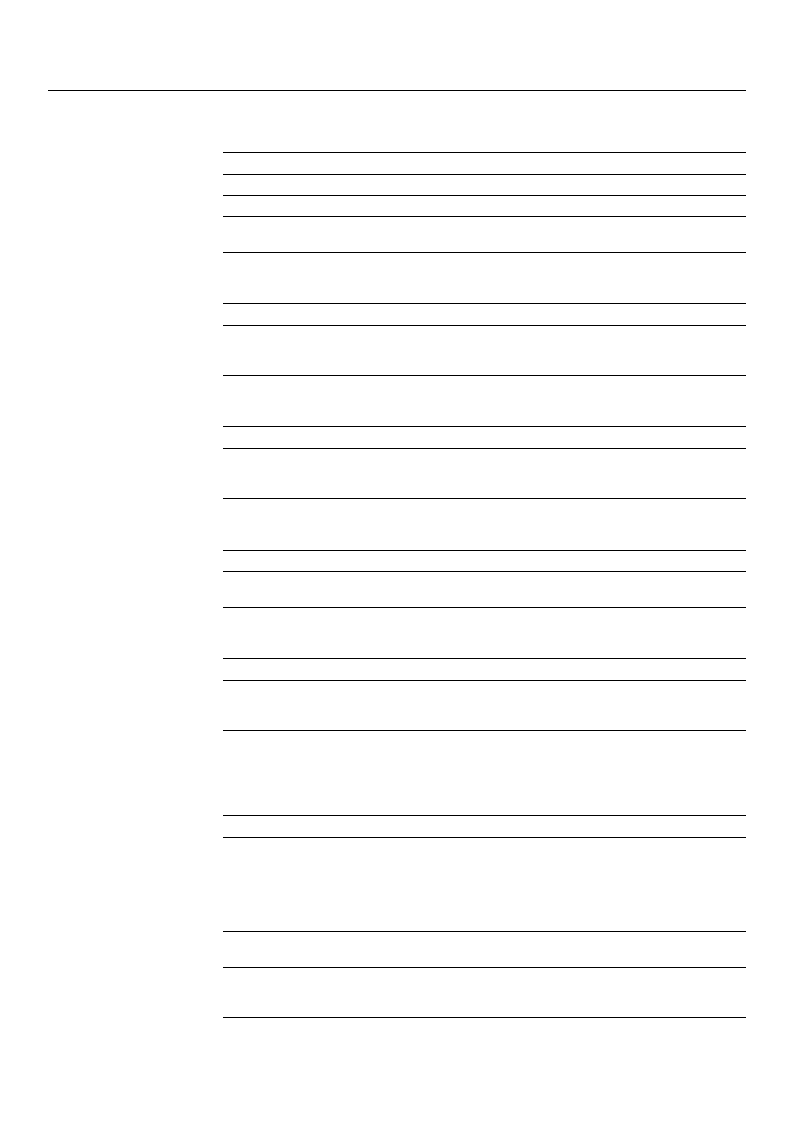
Int. J. Environ. Res. Public Health 2021, 18, 1770
33 of 38
Table A6. EBSCO.
No.
Search Strings
S3
(S1 AND S2)
S2
review* OR systematic* OR overview* OR Meta-Analys*
S1
“forest therap*” OR “forest bath*” OR “forest medicine” OR
“shinrin-yoku” OR “forest healing”
Hits
2
776,703
12
Table A7. CiNii.
No.
Search Strings
Hits
(forest therap* OR forest bath* OR forest medicine OR Shinrin-Yoku OR
1
forest healing) AND (review* OR systematic* OR overview* OR
21
Meta-Analys*)
Table A8. Scopus.
No.
Search Strings
Hits
(TITLE-ABS-KEY(“forest therap*” OR “forest bath*” OR “forest medicine”
1
OR “shinrin-yoku” OR “forest healing”)AND TITLE-ABS-KEY(review* OR
31
systematic* OR overview* OR meta-analys*))
Table A9. Google Scholar.
No.
Search Strings
1
review AND [“forest therapy” OR “forest bathing” OR “forest medicine”
OR “shinrin-yoku” OR “forest healing” -doi]
Hits
1090
Table A10. PROSPERO.
No.
Search Strings
Hits
(“forest therap*” or “forest bath*” or “forest medicine” or “shinrin-Yoku”
1
or “forest healing”) AND (review* or systematic* or overview* or
8
“Meta-Analys*”)
Appendix B.
Table A11. Excluded references after full text analysis.
Reference
Ambrose-Oji, B. Mindfulness Practice in Woods and Forests: An
Evidence Review. Research Report for The Mersey Forest, Forest
Research. Alice Holt Lodge Farnham, Surrey; 2013. Available from:
https://infta.net/files/references/Mindfulness%20and%20
Woods%20Evidence%20Review%20%202013.pdf [Access Date:
6 October 2020].
Cho, K. S.; Lim, Y. R.; Lee, K.; Lee, J.; Lee, J. H.; Lee, I. S. Terpenes
from Forests and Human Health. Toxicol. Res. 2017;33(2):97–106.
Cho, Y.-M.; Kim, D.-J.; Lee, K. H.; Lee, H. E.; Lee, Y. J. A Study on
Effect of Forest Related Programs based on the Meta-Analysis.
Journal of the Korean Institute of Forest Recreation, 2015. 19(1): 1–13.
Reason for Exclusion
No systematic review
No systematic review
No systematic review
Int. J. Environ. Res. Public Health 2021, 18, 1770
34 of 38
Table A11. Cont.
Reference
Karjalainen, E., Sarjala, T. & Raitio, H. Promoting human health
through forests: overview and major challenges. Environ Health Prev
Med. 2010;15:1–8.
Li, Q. Effect of forest bathing trips on human immune function.
Environ Health Prev Med. 2010;15:9–17.
Li, Q. Effect of forest bathing (shinrin-yoku) on human health: A
review of the literature. Santé Publique. 2019;31:135–143.
Li, Q.; Kawada, T. Possibility of Clinical Applications of Forest
Medicine. Japanese Journal of Hygiene. 2014;69(2):117–121.
Meyer, K.; Burger-Arndt, R. How forests foster human
health—Present state of research-based knowledge (in the field of
Forests and Human Health). International Forestry Review.
2014;16(4):421–446.
Meyer-Schulz, K.; Burger-Arndt, R. Une revue de la littérature
scientifique Reviewing the psychological and physical health effects
of forests. Santé Publique. 2019; 31:115–134.
Miyazaki, Y.; Ikei, H.; Song, C. Forest medicine research in Japan.
Japanese Journal of Hygiene. 2014; 69(2):122–135.
Payne, M.; Delphinus, E. The most natural of natural therapies: A
review of the health benefits derived from Shinrin-Yoku (Forest
Bathing). The International Journal of Health, Wellness, and Society.
2019;9:19–30.
Shin, W. S.; Yeoun, P. S.; Yoo, R. W.; Shin, C. S. Forest experience and
psychological health benefits: The state of the art and future prospect
in Korea. Environ Health Prev Med. 2010; 15:38–47.
Zhang, Z. Y.; Wang, P.; Gao, Y.; Ye, B. Current Development Status of
Forest Therapy in China. Healthcare (Basel). 2020;8(1):61.
Corazon, S. S.; Sidenius, U.; Poulsen, D. V.; Gramkow, M. C.;
Stigsdotter, U. K. Psycho-Physiological Stress Recovery in Outdoor
Nature-Based Interventions: A Systematic Review of the Past Eight
Years of Research. Int. J. Environ. Res. Public Health. 2019; 16, 1711.
Haluza, D.; Schonbauer, R.; Cervinka, R. Green Perspectives for
Public Health: A Narrative Review on the Physiological Effects of
Experiencing Outdoor Nature. Int. J. Environ. Res. Public Health.
2014;11,:5445–5461.
Hansen, M. M.; Jones, R.; Tocchini, K. Shinrin-Yoku (Forest Bathing)
and Nature Therapy: A State-of-the-Art Review. Int. J. Environ. Res.
Public Health. 2017;14 (8):851.
Hossain, M., Sultana, A., Ma, P., Fan, Q., Sharma, R., Purohit, N., &
Sharmin, D. F. (2020, January 8). Effects of natural environment on
mental health: an umbrella review of systematic reviews and
meta-analyses. Available from: https://psyarxiv.com/4r3mh/
[Access Date: 6 October 2020].
Kamioka H, Tsutani K, Mutoh Y, Honda T, Shiozawa N, Okada S,
Park SJ, Kitayuguchi J, Kamada M, Okuizumi H, Handa S. A
systematic review of randomized controlled trials on curative and
health enhancement effects of forest therapy. Psychol Res Behav
Manag. 2012;5:85–95.
Reason for Exclusion
No systematic review
No systematic review
No systematic review
No systematic review
No systematic review
No systematic review
No systematic review
No systematic review
No systematic review
No systematic review
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
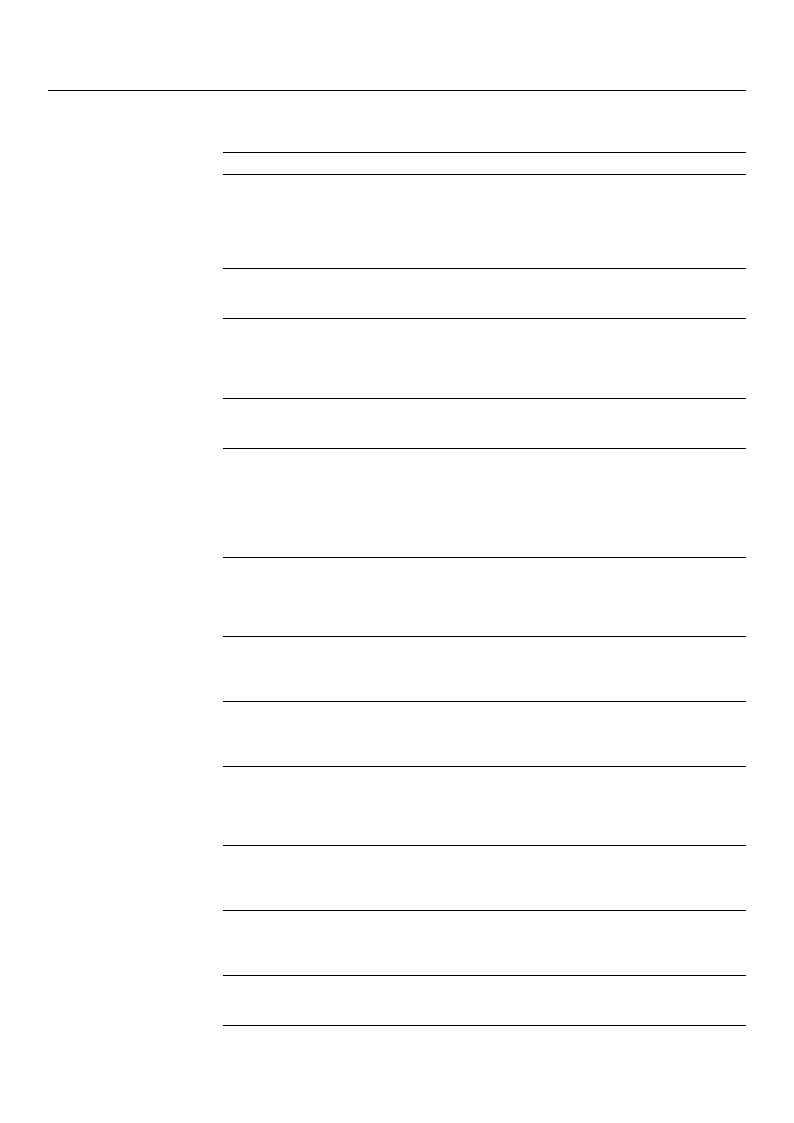
Int. J. Environ. Res. Public Health 2021, 18, 1770
35 of 38
Table A11. Cont.
Reference
Poulsen, D. V. (2015). How war veterans with post-traumatic stress
disorder experience nature-based therapy in a forest therapy garden.
Københavns Universitet: Department of Geosciences and Natural
Resource Management, Faculty of Science, University of Copenhagen.
Available from: https://ign.ku.dk/phd-forsvar/2015/phd-defence-
dorthe-varning-poulsen/ [Access Date: 6 October 2020].
Kim T, Song B, Cho KS, Lee IS. Therapeutic Potential of Volatile
Terpenes and Terpenoids from Forests for Inflammatory Diseases. Int
J Mol Sci. 2020;21(6):2187.
Mathias, S., Daigle, P., Dancause, K. N., & Gadais, T. (2019, December
5). Forest bathing: a narrative review of the effects on health for
outdoor and environmental education use in Canada. Available from:
https://doi.org/10.31236/osf.io/j6mq3 [Access Date:
6 October 2020].
McMahan, E. A.; Estes, D. The effect of contact with natural
environments on positive and negative affect: A meta-analysis. The
Journal of Positive Psychology. 2015;10(6): 507–519.
Meredith Genevive R., Rakow Donald A., Eldermire Erin R. B.,
Madsen Cecelia G., Shelley Steven P., Sachs Naomi A. Minimum
Time Dose in Nature to Positively Impact the Mental Health of
College-Aged Students, and How to Measure It: A Scoping Review.
2020;10:2942 Available from:
https://doi.org/10.3389/fpsyg.2019.02942 [Access Date:
6 October 2020].
Muranen, Anni-Tuulia; Alihanka, Karoliina. Green Exercise in
Supportin the Mental Health of Cardiac patients. Thesis. 2019.
Available from: https://www.theseus.fi/bitstream/handle/10024/26
5719/Muranen_Anni-Tuulia%2C%20Alihanka_Karoliina.pdf?
sequence=2&isAllowed=y [Access Date: 6 October 2020].
Mygind L, Kjeldsted E, Hartmeyer R, et al.. Effects of Public Green
Space on Acute Psychophysiological Stress Response: A Systematic
Review and Meta-Analysis of the Experimental and
Quasi-Experimental Evidence. Environment and Behavior. 2019.
Mygind L, Kjeldsted E, Hartmeyer RD, Mygind E, Bølling M, Bentsen
P. Immersive Nature-Experiences as Health Promotion Interventions
for Healthy, Vulnerable, and Sick Populations? A Systematic Review
and Appraisal of Controlled Studies. Front Psychol. 2019;10:943.
Nilsson K, Bentsen P, Grahn P, Mygind L. De quelles preuves
scientifiques disposons-nous concernant les effets des forêts et des
arbres sur la santé et le bien-être humains ? [What is the scientific
evidence with regard to the effects of forests, trees on human health
and well-being?]. Sante Publique. 2019;S1(HS):219–240. French.
Roberts H, van Lissa C, Hagedoorn P, Kellar I, Helbich M. The effect
of short-term exposure to the natural environment on depressive
mood: A systematic review and meta-analysis. Environ Res.
2019;177:108606.
Roth, A.-S. (2011). Naturen—En resurs för stressåterhämtning: En
systematisk litteraturstudie (Dissertation). Available from:
http://urn.kb.se/resolve?urn=urn:nbn:se:his:diva-5342 [Access Date:
6 October 2020].
Sun, Seung-Ho; Lee, Seon-Goo. Systemic review on forest healing
journals. Korean J. Oriental Physiology & Pathology 2010; 24(4):
566–570.
Reason for Exclusion
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
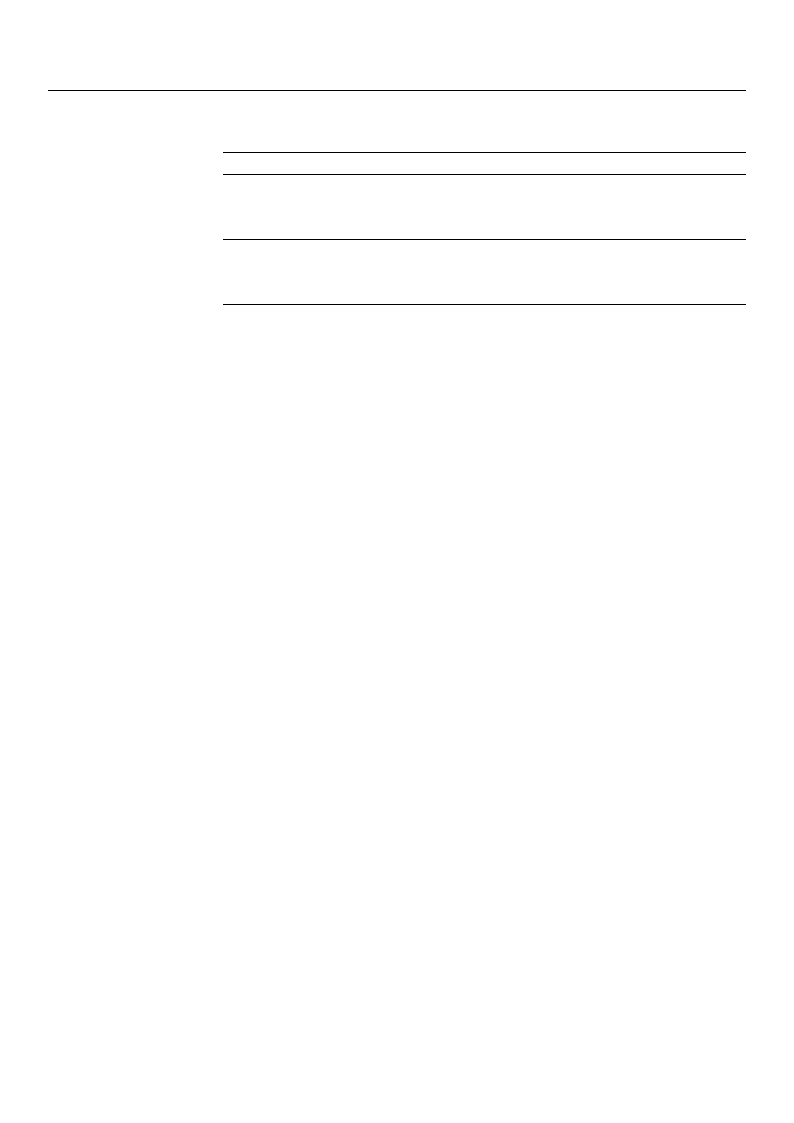
Int. J. Environ. Res. Public Health 2021, 18, 1770
36 of 38
Table A11. Cont.
Reference
Twohig-Bennett, Caoimhe; Jones, Andy. The health benefits of the
great outdoors: A systematic review and meta-analysis of greenspace
exposure and health outcomes. Environmental Research. 2018,
166:628–637.
Vibholm, A. P.; Christensen, J. R.; Pallesen, H. Nature-based
rehabilitation for adults with acquired brain injury: a scoping review.
International Journal of Environmental Health Research, 30:6,
661–676.
Reason for Exclusion
Non-predominant forest
(≥80% of the studies)
Non-predominant forest
(≥80% of the studies)
Appendix C. Deviation from the AMSTAR-2 Guidance Document
We have made the following adjustments for the quality assessment of the current
SRs and MAs:
1. Many items in the AMSTAR-2 can be answered with “Partial Yes” or “Yes”. Several
criteria must usually be met for a “Partial Yes”. The criteria for “Partial Yes” and
several additional criteria must be met for a “Yes”. This is usually formulated as
“For Yes should also have...” or “For Yes must also have...”. We have interpreted and
applied these rules as follows: for a formulation with “should”, at least one of the
following criteria had to be met for a “Yes”, and all the criteria listed had to be met
for a formulation with “must”.
2. Item 4: “Did the review authors use a comprehensive literature search strategy?”
Three criteria must be met for a “Partial Yes” to this question. One of them is “justified
publication restrictions (e.g., language)”. Since the restrictions for the literature search
are usually described, but only very rarely justified, we did not take this criterion into
account in the evaluation.
3. Item 7: “Did the review authors provide a list of excluded studies and justify the
exclusions?” For a “Yes” to this question, a list of the excluded studies must be
available, and the exclusion of every potentially relevant study from the review must
be justified. The evaluation was modified as follows: for a “Yes”, it was sufficient if
the number of excluded studies and information about how many studies had been
excluded for what reasons in the paper (e.g., in PRISMA Flow Chart) were listed.
References
1. United Nations. Department of Economic and Social Affairs (UN/DESA): World Urbanization Prospects: The 2018 Revision.
Available online: https://population.un.org/wup/Publications/Files/WUP2018-KeyFacts.pdf (accessed on 27 November 2020).
2. Corazon, S.S.; Sidenius, U.; Poulsen, D.V.; Gramkow, M.C.; Stigsdotter, U.K. Psycho-Physiological Stress Recovery in Outdoor
Nature-Based Interventions: A Systematic Review of the Past Eight Years of Research. Int. J. Environ. Res. Public Health
2019, 16, 1711. [CrossRef]
3. Hansen, M.M.; Jones, R.; Tocchini, K. Shinrin-yoku (forest bathing) and nature therapy: A state of the art review. Int. J. Environ.
Res. Public Health 2017, 14, 851. [CrossRef]
4. Twohig-Bennett, C.; Jones, A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace
exposure and health outcomes. Environ. Res. 2018, 166, 628–637. [CrossRef] [PubMed]
5. Bowler, D.E.; Buyung-Ali, L.M.; Knight, T.M.; Pullin, A.S. A systematic review of evidence for the added benefits to health of
exposure to natural environments. BMC Public Health 2010, 10. [CrossRef]
6. Li, Q. Effect of forest bathing trips on human immune function. Environ. Health Prev. Med. 2010, 15, 9. [CrossRef] [PubMed]
7. Markov, S.; Steckenbauer, G.C.; Pillmayer, M.; Herntrei, M. Austria: The Forest as a Touristic Landscape. In International
Handbook of Forest Therapy; Kotte, D., Li, Q., Shin, W.S., Michalsen, A., Eds.; Cambridge Scholars Publishing: Newcastle, UK, 2019;
pp. 337–355.
8. Li, Q. Forest Medicine—Public Health in the 21st Century; Nova Science Publisher: New York, NY, USA, 2012.
9. Kotte, D.; Li, Q.; Shin, W.S.; Michalsen, A. International Handbook of Forest Therapy; Cambridge Scholars Publishing: Newcastle,
UK, 2019.
10. Li, Q. What is Forest Medicine? In Forest Medicine; Nova Science Publisher: New York, NY, USA, 2013.
11. Schuh, A.; Immich, G. Waldtherapie—Das Potential des Waldes für Ihre Gesundheit; Springer-Verlag: Berlin/Heidelberg,
Germany, 2019.

Int. J. Environ. Res. Public Health 2021, 18, 1770
37 of 38
12. Kaiserbaeder Usedom. Cure and Healing Forests. 2002. Available online: https://www.kur-und-heilwald.de/?lang=en
(accessed on 12 December 2002).
13. Karim, A.; Khalil, R.; Schmitt, M. Wald reloaded—Die Neuentdeckung des Waldes aus gesundheitspsychologischer Sicht.
Z. Komplementärmedizin 2020, 2, 24–30. [CrossRef]
14. Vukin, M.; Isailovic´, G. A Cure and Healing Foest of Gocˇ Mountain—A New Approach to Health Tourism in Serbia.
Available online: https://de.calameo.com/read/00586528821d0b12eaa9b (accessed on 22 November 2020).
15. Berman, M.G.; Jonides, J.; Kaplan, S. The cognitive benefits of interacting with nature. Psychol. Sci. 2008, 19, 1207–1212. [CrossRef]
16. Peen, J.; Schoevers, R.A.; Beekman, A.T.; Dekker, J. The current status of urban-rural differences in psychiatric disorders. Acta
Psychiatr. Scand. 2010, 121, 84–93. [CrossRef]
17. Van Den Berg, A.E.; Maas, J.; Verheij, R.A.; Groenewegen, P.P. Green space as a buffer between stressful life events and health.
Soc. Sci. Med. 2010, 70, 1203–1210. [CrossRef]
18. Müllner, M. Epidemiologie der Zivilisationskrankheiten. In Bewegung als Therapie: Gezielte Schritte zum Wohlbefinden;
Zwick, H., Ed.; Springer Verlag: Wien, Austria, 2007; pp. 13–31.
19. Oh, B.; Lee, K.J.; Zaslawski, C.; Yeung, A.; Rosenthal, D.; Larkey, L.; Back, M. Health and well-being benefits of spending time in
forests: Systematic review. Environ. Health Prev. Med. 2017, 22. [CrossRef] [PubMed]
20. Vibholm, A.P.; Christensen, J.R.; Pallesen, H. Nature-based rehabilitation for adults with acquired brain injury: A scoping review.
Int. J. Environ. Health Res. 2020, 30, 661–676. [CrossRef]
21. Meyer, K.; Burger-Arndt, R. How forests foster human health—Present state of research-based knowledge (in the field of Forests
and Human Health). Int. For. Rev. 2014, 16, 421–446. [CrossRef]
22. Meyer-Schulz, K.; Burger-Arndt, R. Reviewing the Psychological and Physical Health Effects of Forests. Santé Publique 2019, 31
(Suppl. S1), 115–134. [CrossRef]
23. Stier-Jarmer, M.; Throner, V.; Kirschneck, M.; Frisch, D.; Schuh, A. Psychological and Physical Effects of Forests on Human Health—A
Systematic Review of Systematic Reviews and Meta-Analyses; 2020; Available online: https://www.crd.york.ac.uk/prospero/display_
record.php?ID=CRD42020190649 (accessed on 11 February 2021).
24. Stern, C.; Jordan, Z.; McArthur, A. Developing the Review Question and Inclusion Criteria. Am. J. Nurs. 2014, 114, 53–56.
[CrossRef]
25. Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al.
AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare
interventions, or both. BMJ 2017, 358, j4008. [CrossRef] [PubMed]
26. Cochrane Deutschland Stiftung, Institut für Evidenz in der Medizin, Institut für Medizinische Biometrie und Statistik, Freiburg,
Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften, Institut für Medizinisches Wissensmanagement,
Ärztliches Zentrum für Qualität in der Medizin. Manual Systematische Recherche für Evidenzsynthesen und Leitlinien. 2019.
Available online: https://freidok.uni-freiburg.de/data/149324 (accessed on 20 November 2020). [CrossRef]
27. Antonelli, M.; Barbieri, G.; Donelli, D. Effects of forest bathing (shinrin-yoku) on levels of cortisol as a stress biomarker: A
systematic review and meta-analysis. Int. J. Biometeorol. 2019, 63, 1117–1134. [CrossRef] [PubMed]
28. Ideno, Y.; Hayashi, K.; Abe, Y.; Ueda, K.; Iso, H.; Noda, M.; Lee, J.S.; Suzuki, S. Blood pressure-lowering effect of Shinrin-yoku
(Forest bathing): A systematic review and meta-analysis. BMC Complement. Altern. Med. 2017, 17, 409. [CrossRef] [PubMed]
29. Kotera, Y.; Richardson, M.; Sheffield, D. Effects of Shinrin-Yoku (Forest Bathing) and Nature Therapy on Mental Health: A
Systematic Review and Meta-Analysis. Int. J. Ment. Health Addict. 2020. [CrossRef]
30. Farrow, M.R.; Washburn, K.A. Review of Field Experiments on the Effect of Forest Bathing on Anxiety and Heart Rate Variability.
Glob. Adv. Health Med. 2019, 8. [CrossRef]
31. Lee, I.; Bang, K.S.; Kim, S.; Choi, H.; Lee, B.; Song, M. Effect of Forest Program on Atopic Dermatitis in Children—A Systematic
Review. J. Korean Inst. For. Recreat. 2016, 20, 1–13. [CrossRef]
32. Lee, I.; Choi, H.; Bang, K.S.; Kim, S.; Song, M.; Lee, B. Effects of forest therapy on depressive symptoms among adults: A
systematic review. Int. J. Environ. Res. Public Health 2017, 14, 321. [CrossRef]
33. Putra, R.R.F.A.; Veridianti, D.D.; Nathalia, E.; Brilliant, D.; Rosellinny, G.; Suarez, C.G.; Sumarpo, A. Immunostimulant Effect
from Phytoncide of Forest Bathing to Prevent the Development of Cancer. Adv. Sci. Lett. 2018, 24, 6653–6659. [CrossRef]
34. Song, M.K.; Bang, K.-S. A systematic review of forest therapy programs for elementary school students. Child Health Nurs. Res.
2017, 23, 300–311. [CrossRef]
35. Chae, Y.R.; Kim, J.H.; Kang, H. Literature Review of Forest Healing Therapy on Korean Adults. J. Korean Biol. Nurs. Sci. 2018, 20,
122–131. [CrossRef]
36. Wen, Y.; Yan, Q.; Pan, Y.; Gu, X.; Liu, Y. Medical empirical research on forest bathing (Shinrin-yoku): A systematic review. Environ.
Health Prev. Med. 2019, 24, 70. [CrossRef] [PubMed]
37. Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and
Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [CrossRef] [PubMed]
38. Pieper, D.; Antoine, S.-L.; Mathes, T.; Neugebauer, E.A.M.; Eikermann, M. Systematic review finds overlapping reviews were not
mentioned in every other overview. J. Clin. Epidemiol. 2014, 67, 368–375. [CrossRef] [PubMed]
39. Yau, K.K.-Y.; Loke, A.Y. Effects of forest bathing on pre-hypertensive and hypertensive adults: A review of the literature. Environ.
Health Prev. Med. 2020, 25, 23. [CrossRef] [PubMed]

Int. J. Environ. Res. Public Health 2021, 18, 1770
38 of 38
40. Grilli, G.; Sacchelli, S. Health Benefits Derived from Forest: A Review. Int. J. Environ. Res. Public Health 2020, 17, 6125. [CrossRef]
[PubMed]
41. Hansen, M.M.; Jones, R. The Interrelationship of Shinrin-Yoku and Spirituality: A Scoping Review. J. Altern. Complement. Med.
2020, 26, 1093–1104. [CrossRef] [PubMed]
42. Rajoo, K.S.; Karamb, D.S.; Abdullaha, M.Z. The physiological and psychosocial effects of forest therapy: A systematic review.
Urban For. Urban Green. 2020, 54, 126744. [CrossRef]
43. Kang, M.-J.; Myung, S.-K. Effects of Forest-Based Interventions on Mental Health; A Meta-Analysis of Randomized Controlled
Trials. 2020. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020202489 (accessed on
11 February 2021).
44. Ioannou, S.; Patterson, L.; Whittaker, P. The Health Benefits of Forest Therapy: An Umbrella Review. 2019. Available online:
https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019136586 (accessed on 11 February 2021).
45. Kemper, H. Waldbaden: Der Wald Wirkt Entschleunigend; ZEIT Wissen: Hamburg, Germany, 2018; p. 3.
46. Markert, R. Alternative Medizin. Waldtherapie—Gesund durch Natur? 2019. Available online: https://www.zdf.de/nachrichten/
heute/alternative-medizin-heilung-durch-waldtherapie-100.html (accessed on 28 October 2020).
47. Abe, T.; Hisama, M.; Tanimoto, S.; Shibayama, H.; Mihara, Y.; Nomura, M. Antioxidant effects and antimicrobial activites of
phytoncide. Biocontrol. Sci. 2008, 13, 23–27. [CrossRef] [PubMed]
48. Li, Q.; Morimoto, K.; Kobayashi, M.; Inagaki, H.; Katsumata, M.; Hirata, Y.; Hirata, K.; Suzuki, H.; Li, Y.J.; Wakayama, Y.; et al.
Visiting a forest, but not a city, increases human natural killer activity and expression of anti-cancer proteins. Int. J. Immunopathol.
Pharmacol. 2008, 21, 117–127. [CrossRef]
49. Šimpraga, M.; Ghimire, R.P.; Van Der Straeten, D.; Blande, J.D.; Kasurinen, A.; Sorvari, J.; Holopainen, T.; Adriaenssens, S.;
Holopainen, J.K.; Kivimaenpaa, M. Unravelling the functions of biogenic volatiles in boreal and temperate forest ecosystems.
Eur. J. For. Res. 2019, 138, 763–787. [CrossRef]
50. Antonelli, M.; Donelli, D.; Barbieri, G.; Valussi, M.; Maggini, V.; Firenzuoli, F. Forest Volatile Organic Compounds and Their
Effects on Human Health: A State-of-the-Art Review. Int. J. Environ. Res. Public Health 2020, 17, 6506. [CrossRef]
51. Park, B.J. Forest Welfare Policy in South Korea. Poster Präsentation am 2. In Proceedings of the Internationalen Kongress
„Gesundheitspotential Wald“, Krems, Austria, 6–7 November 2018.
52. Clifford, A. Your Guide to Forest Bathing; Conari Press: Newburyport, MA, USA, 2018.
53. Imai, M. An introduction to the Forest Therapy Society of Japan, Forest Therapy and Forest Therapist. In Forest Medicine;
Li, Q., Ed.; Nova Science Publishers: Hauppauge, NY, USA, 2012.
54. Kang, B.; Kim, T.; Kim, M.J.; Lee, K.H.; Choi, S.; Lee, D.H.; Kim, H.R.; Jun, B.; Park, S.Y.; Lee, S.J.; et al. Relief of chronic posterior
neck pain depending on the type of forest therapy: Comparison of the therapeutic effect of forest bathing alone versus forest
bathing with exercise. Ann. Rehabil. Med. 2015, 39, 957–963. [CrossRef] [PubMed]
